NOTE – I am not a doctor. Please consult with your physician before trying anything. This is merely an account of my story.
Still, I won’t lie. I had a difficult experience. I don’t think it’s that way for everyone. In addition to the physical challenge, it can be a mental challenge and, for me, it lead to other things, like an eating disorder and mental fatigue. According to my doctor, these problems are pretty common.
In fact, he said, it can be so psychologically and physically challenging that in Canada they have an entire institute that’s dedicated to helping people with the different aspects of this issue. It’s called the RUDD CLINIC. I’m not affiliated with it but I thought I’d pass along their info in case it helped:
http://ruddclinic.com/patientinfo01.html
http://ruddclinic.com/resources.html
He said that’s it’s normal that it takes long to heal, from 6 months to a year. My healing process due to complications took about 12 months. It was a challenge but, like I said, you will get through it. Here’s my story. Hopefully, there’s some info in it that will prove helpful:
AT THE END OF APRIL…
-My stool became hard. It was the result of my unhealthy habits (constipating food, excessive alcohol, stress, etc). To pass it, I kept straining. This was over several days, then one time I strained too much and I injured myself. I felt something give. There was blood and I developed a fissure. (Also, I had a chronic hemorrhoid and a polyp) I waited two weeks before seeing my primary care doctor. It got worse. When I finally saw him, he recommended:
- -SITZ BATH - I should sit in a warm tub of water, twice a day, for about 5 to 10 minutes. Nothing super hot. Just warm. This helps put pressure on the hemroids and pushes them back in.
- MORE FIBER - I should take Citracel rather than Metamucil. It’s better. Adding fiber will help retain water in my stool and make it softer to pass.
- SUPPOSITORY - He gave me a prescription for a suppository. I should take it for a week only at bedtime. If it’s not better after the suppositories and the treatments, I need to come back and have it scoped so they can find out what it is.
- AVOID OATMEAL – Sometimes, it can constipate
- AVOID TUCKS – It has witch hazel in it.
- AVOID BABY WIPES
I tried these things but the situation only got worse. I passed progressively more blood and ended up in Urgent Care. They sent me back to my primary care doctor who recommended I visit a colorectal surgeon:
THE COLORECTAL SURGEON
I needed to get in quickly. My primary care doctor recommended that I tell them that I’m in a lot of pain and I need to see the surgeon right away. I did and the colorectal surgeon saw me the next morning.
He recommended the following.
SITZ BATH:
-When I have a BM (bowel movement), I should wipe with soft toilet paper
-Then, I should take a lukewarm sitz bath afterward for about 10 to 15 minutes
-Then, when I got out, I should dab it with a paper towel (I shouldn’t let it air dry)
DILTIAZEM OINTMENT
-After the bath, at least twice a day, I should apply a DILTIAZEM ointment.
To apply
-I put on a latex glove,
-Cover the tip of my index finger up to the first knuckle with ointment,
-Then insert the index finger into my rectum all the wall up to the first knuckle
-Gently rub the ointment back and forth once (since it’s an ointment, it doesn’t get absorbed. You don’t have to over rub)
-Then, as I pull the index finger out, rub the ointment again on the opening of the rectum
-I should do this twice a day
-After two to three weeks, I can do this once a day
Regarding the ointment:
-It’s a special ointment. I have to go to a compounding pharmacy to get it. They make it there.
-You might have to call the compounding pharmacist the day before so they can get it ready. (Luckily, the first time I went they just happened to have an extra one on hand)
-You should keep it at room temperature.
-You shouldn’t rub it. You should apply it just once. It’s not going anywhere and rubbing it might just irritate it
Ointment Purpose
It’s to get blood down there and help with the healing. It’s also relaxes/loosens things up and helps with the spasms
SPASMS
I developed involuntary spasms in the rectal area. My body would slowly clench up my sphincter and then slowly release it, over and over and over again, all night long. My doctor said that the fissure had created a lack of tension down there and that my body was trying to fix this problem by clenching up and creating tension. Unfortunately, it was clenching up right where the fissure pain was located. I followed the doctor’s advice and applied the DILTIAZEM ointment twice a day. It helped and the spasms eventually went away. I won’t lie. The spasms were a challenge but I got through them. It was a mental battle, too. You need to do things to focus your mind elsewhere. Breathing deeply, repeating positive sayings, etc. really got me through it.
CONSTIPATION - PASSING HARD STOOL THROUGH A SMALL OPENING
I encountered an issue where I would get the urge for a BM. My bowels would attempt to move but the BM wouldn’t be able to pass through the opening (possibly because the opening had swollen, making it smaller than usual). So, an hour later, my body would spasm again and again, it would try to pass the stool without success. I didn’t want to strain since that brought about the fissure in the first place. So instead, I would just suffer through it until eventually the BM would pass (Sometimes many hours later). (Taking a deep breath and holding it seemed to help because it stretched my torso and pressured the bowel)
Also, according to my nutritionist, stress can cause hard stool, too. She did a little illustration pointing out that there’s little gate keepers in your rectum. When you get stressed, they lock up – and they make the stool very hard to pass. She seems to think this might have been happening when I had those spasm days. She really emphasized the point that the mind controls the whole body. If it’s stressed, it locks everything up down there. As a result, stool would get hard.
In hindsight, I should’ve gotten a stool softener at the pharmacy (like MiraLAX) and that probably would’ve helped (although it might take a couple of days for it to take effect). My anxiety was also causing problems and causing the stool to pass slower through my system. Once I got on anti-anxiety medication, it seemed to help (This takes a little bit of time to take effect too). These days, I’m recovered. The fissure is healed. I don’t take stool softener or anti-anxiety medication. I do drink plenty of water to keep the stool soft. Also, before I go to bed each night, I drink a little bit of prune juice. The sugar in prune juice helps retain moisture in the stool and keeps it soft. When I wake up in the morning, I’ll drink a glass of water and, about fifteen minutes later, I’ll have a healthy BM. Again, if you’re having trouble passing stool, ask your doctor if you should try a stool softener (like MiraLAX. You can buy it off the counter). Sometimes doctors don’t think of these things. I didn’t know they were out there. I wish I had.
Regarding adding more fiber to my diet…
CITRACEL
It’s a fiber supplement. It should help your stool retain water and make it soft. When you take it, you should make sure it’s been dissolved throughout the glass, then after you drink it, you should drink another glass of water (Citracel can constipate too if it’s not used properly)
WEIGHT LOSS
-Due to the pain while passing stool, I had drastically cut back on eating. As a result, I developed an eating disorder and lost a lot of weight. Not a good thing. If I was going to get over this thing, I would need to be healthy. Instead, I looked gaunt and weak. I saw my primary care physician about it and he told me to resume eating everything, especially fruits and vegetables. He says that if you fast too long you’ll get constipated and when you finally have a bowel movement it will blow away everything. Eventually, I took action and asked my primary care doctor to recommend a certified nutritionist. I visited her and she tailored a diet for me that really helped. I needed to put on weight. So, she created a diet with healthy fats. Unfortunately, she didn’t tell me to ease into it. My body tried to reject the sudden increase in fat and I got diarrhea. Once I dialed things back and eased into the new diet, things were fine and I eventually put on weight. If you are dealing with weight loss and fear of eating due to a fissure, I would highly recommend seeing a nutritionist. It helped me. (More on that later)
___
Regarding the fissure, I tried the DILTIAZEM routine for about a month and a half. I kept wavering between getting good and getting bad. I kept reinjuring the fissure due to hard stool.
I would need to get surgery after all. It was decided to schedule…
SURGERY – lateral internal sphincterotomy and a hemoroidectomy
TIME AWAY
-With my employer, I had to set up my time away from work. I would be on short term disability. They told me that I might want to take a full month off work.
ABOUT A WEEK PRIOR
I went to the medical center where my surgery would be performed and I had a PRE-REGISTRATION session. Basically, I did a bunch of paperwork, gave some contact info regarding who would be helping me and a nurse took my readings and answered my questions.
FIVE DAYS PRIOR TO SURGERY
PRE-OP
-I went to my primary care physician and got a PRE-OPERATIVE CONSULTATION. (This was requested by my colo-rectal surgeon)
On the night before the consultation, I would start fasting – no food. Then, the day of the tests, I could drink water only. They would take a bunch of tests (blood, EKG, X-Ray, etc) then my primary care doctor would go over the results. If they looked good, he would clear me for surgery. (If you need to get a pre-op consultation, set it up RIGHT AWAY. The logistics were a bit tricky. I had my tests done on one day. Then, my doctor looked them over the next day – and then, he had to get the info back to my surgeon and the medical center before the surger. Again, these things take time and they don’t want to do them too far in advance. Plus, trying to find a time to see your doctor on short notice can be difficult. So, set this up right away and allow yourself enough time)
-Also, I called my surgeon to see if I could get the prescription for my post-op pain medication pre-filled. That way, it would be ready to go after my surgery.
TWO DAYS PRIOR
-Stop using the DILTIAZEM OINTMENT.
-Before the surgery, I had to clean out my digestive track. Two days prior to surgery, I started taking COLACE 100mg – TWICE A DAY. It’s a stool softener and it made my stool easier to pass. I will be taking it to primarily avoid constipation from the pain killers.
On the day of my surgery, I shouldn’t take it.
After surgery, I should resume taking COLACE for two weeks.
DAY BEFORE SURGERY
-My doctor didn’t want me to do an enema (Might cause more problems)
-Eat a normal breakfast and lunch
-After 2pm, nothing to eat – stay on a STRICT LIQUID DIET
-After 2pm, I will start drinking GOLYTELY. It’s a powder that comes in a jug. They give you instruction on how to fill it with water, shake it and mix the solution into the water.
-You’re suppose to drink all of it. It’s an instant laxative that causes you to pass everything out of your digestive tract in preparation for surgery.
-I can take 4 hours to drink it. They normally have you do 4 liters. I will drink 2.5 liters. This is about half of what they normally do.
-I will start passing. It will be painful but I have to do it.
-After taking Golytely, don’t take any more Colace stool softener.
-Shower night before
-After midnight, don’t eat or drink anything. No food or water after midnight. Nothing in your mouth. I can brush my teeth but that’s it.
DAY OF SURGERY
Don’t take Colace the day of surgery.
-Wear glasses – no contacts
-Don’t bring valuables
-Wear comfortable clothes & shoes
-Bring insurance card and picture I-D
I was told to get to the surgery center at 7am.
-I will fill out some paperwork (including the surgery order that I’ll okay)
-They’ll take me back. I’ll strip, get in gown. They’ll put me in bed 20, hook me up to heart monitor, give me IV. They’ll wheel me into surgery, put me under at some point and they’ll do the procedure.
Surgery was at9am – 10:30am on a Friday morning. I was in for a half day. (Surgery itself was about an hour)
-Procedure – sphincterotomy and a hemoroidectomy - They cut into the internal sphincter to fix it (Of course on the initial paperwork, they had the wrong procedure written down. Again, go over all your paperwork and double check everything. Follow up and be assertive)
-The surgery went fine. They said they found what they thought was a benign polyp, and they sent it out for a biopsy. They said everything looked good and I should be okay.
-After surgery, they slowly wake you up.
They wanted me to urinate before I left the hospital. I tried a couple of times but I couldn’t urinate. So, they put a catheter in me and drained the urine that way. (Regarding the catheter, Doc said to do it in a half hour. The nurse waited an hour. After that, she finally had to do it.) With the drugs and everything else that I had been through, it wasn’t painful. They drained the urine and sent me home. If I had trouble urinating again, I would need to be catheterized in an ER. Luckily, this didn’t happen.
PROBLEMS TO LOOK FOR POST-SURGERY – Go to the ER if I experience any of the following…
-severe rectal pain/bleeding
-persistent nausea and/ or vomiting
-fever
-chills
-abdominal pain
-chest pain
-shortness of breath
-inability to urinate
-excessive diarrhea
-unable to have a BM for more than 4-5 days
Prior to surgery, I spoke with a nurse and asked the following questions regarding possible post-surgery issues:
DRIVING HOME
-How can I be comfortable? Can I sit?
A: Yes, I can probably sit. Or, I can lay. Pillows may help.
-I have stairs. Any advice on climbing the stairs?
A: Take my time
DRESSING
-Are there stitches? A dressing?
A: Not sure about stitches. The nurse said it might be more of an open wound.
For dressing, I will probably have a pad (almost like a female pad)
-When should I remove the dressing? (12 or 24 hours?)
A: I can take it off whenever I feel comfortable. I might want to leave it there initially. It will act like a buffer between the wound and clothes. I can take it off that night if I want.
-How should I remove the dressing? Is it easy to remove?
A: It sounds like it’s easy to remove and it should just come off.
-How soon can I have a sitz baths in the water? (12 hrs? 24 hrs?)
A: I just take it for comfort. I don’t have to have the pad on when I take the bath. DON’T USE EPSON SALTS – It will draw fluid away from the wound.
Should I do it day of surgery with dressing? Can I get the dressing wet?
-No. (I’ll get a packet with more details) Don’t get it wet.
-Do I need to apply a new dressing? Put in more packing?
-Once it’s off, you don’t need a new one
-How soon can I plan on bathing after surgery?
-I should wait around 2 days after surgery. She said I could probably do it late Saturday or Sunday
STOOL – FIRST ONE
-What can I expect?
-It will be tender and some pain. They’ll give me a spray bottle to use to clean it and I should do sitz baths to relieve pain.
***NOTE*** According to her, on average, it takes 12 hours for food to go from mouth to anus.
-Can I expect blood? How much? For how long?
-I’ll maybe have a little on the tissue or stool. (Having too much would be a bowl of blood. Then, contact the doctor)
-Can I use anal lube in the area to ease the stools?
-She wasn’t too keen on this. If I had to, make sure it was water soluble. Just wash the area with water.
-What should I do after passing stool?
-Dab area and take a sitz bath
-Can I expect SPASMS? What should I do if they occur?
-That’s what the pain pills are for.
SLEEPING
-Is there a preferred position for me to sleep in and sit in? Side? Back? Lay on stomach?
-Whatever’s comfortable. I’ll probably be pretty knocked out the first day.
Should I set an alarm to wake me up to take pain killers?
-She didn’t feel there was a need. My body will wake me when there’s pain. There’s no need to wake up. (Plus, they don’t want me to overdue it and I get constipated)
PAIN KILLERS
Once I take one, I need to wait four hours before taking another, right?
-Yes. They don’t want me to overdue it. (Like with Tylenol, you don’t want to take more than 3000mg a day)
What if pain killers are not working? Can I up the amount?
-Call Doctor and tell him right away
ANAL CREAMS
-Do they recommend a local pain reliever like Amercaine or Nuper Canal?
-Doctor will probably want to try pain pills first. I should ask him. That stuff might be by prescription only
-I’m not taking Colace the day of surgery. When should I resume taking COLACE twice a day?
When I start eating anything other than the clear diet.
CITRUCEL
-I was taking a teaspoon of Citrucel each morning. When should I resume?
-Citrucel only adds fiber. Again, wait til you’re eating and you feel you need fiber.
DIET
-By the day after surgery, can I start switching from clear diet to low residue?
-Sure. Do it gradually. The important thing is they don’t want you to get nauseous. So, do it when you feel you won’t be nauseous and eat whatever you feel won’t make you nauseous.
-When can I add eggs and protein?
-Friday (the day of surgery) is a clear day per Doc. Saturday morning I could eat eggs. Again, just don’t eat too much.
-Incontinence?
It can happen but he’s never had a patient that’s had it afterward
-Complications?
Infection, bleeding, incontinence, etc. (He’s does this all the time. It shouldn’t be an issue)
INFECTION
She didn’t seem to think I have to worry about it. An infection usually takes 4, 5 to 6 days to get going, then it’s foul, green puss and it’s red and tender. (Within that time, I’ll be seeing the Doc. So, he’ll be able to tell)
-If I don’t have a fever, I shouldn’t worry.
-The fact that’s it’s a bit swollen, changing shape and draining clear liquid and some red is fine and it’s normal. It’s also good that I don’t have any pain.
END OF NURSE NOTES
-After surgery, I need to stay with someone for 2 to 3 days. They don’t expect anything but just in case I pass out, there’s someone to call 911.
THE AFTERNOON/NIGHT AFTER SURGERY
PAIN MEDICATION - HYDROCODONE
My doctor said I would experience the most pain following the first couple of days post-surgery. After that, it should subside.
During the surgery, they administered some pain medication which would last about 4 hours, then I was instructed to start HYDROCODONE (which is the generic name for VICODIN). They said it was okay to take the stool softener with the Hydrocodone, as Hydrocodone causes constipation and the two together will alleviate issues.
-I should take it at first twinge of pain. Don’t wait for a lot of pain or you won’t be able to bring your pain level back down. Take when I start to feel pain.
-Take pain medication every 4 to 6 hours. I don’t have to be militant about taking it every 4 to 6 hours. Just don’t take two within four hours.
-I should take them as needed. If the pain isn’t as much, I can cut back.
-I should eat food before I take it. (Jello is fine. I just need something in my stomach)
-In the prescription, they gave me 40 pills
(Need 42 pills for one week, 84 for two weeks if taking every 4 hours)
If I need more, they can give me more in the follow up.
-I should avoid aspirin and ibuprofen.
-Digestion – The anesthetic and pain killers will slow down my digestion and make it harder to pass stool. That’s why the doctor wants to me to start out with a clear diet then graduate to low residue foods diet. (And it helps being cleared out the night before)
-After surgery, I wasn’t really in pain. I was taking the pain killers every four hours. On Sunday, I tried stretching it to five hours (but over night I did 4 hours)
Turns out, I didn’t really have an issue. I guess, the pain medication really did the trick. I never really felt much pain post surgery.
-After surgery, I resumed taking COLACE twice a day. I should continue doing this for two more weeks. It combats against the constipation caused by the pain killers.
PACKING
After surgery, I had lots of packing over the wound. I was told to keep it there until my first urge for a BM. Then, I could untape it and remove it. (They said if I didn’t have a bowel movement in a couple of days I could try prune juice. Again, luckily I didn’t need to)
-Friday night (the night after my surgery) around 9pm, I felt like I was going to pass a BM. I decided to pull out the gauze. This was about a foot long and bloody. Instead of passing stool, I passed a whole bunch of water, which I suspected was left over Golytely. After that, I seemed to be incontinent. I would get the urge to pass and I would start squirting water out my butt. There was blood with this at first. Then, mid-day Saturday (the day after surgery), it slowed to just clear drainage with light colored blood.
-My anus had swollen and it changed shape over time.
-Sunday night, after I did a sitz bath, the upper left of the anus seemed to be a bit red and swollen. (I consulted with a told me to stop looking at it. It would turn out later that this had been infected.)
DIET
-Friday, post surgery, I was on a clear diet (lots of liquids basically). Avoid citrus and spicy foods.
-Then, I could gradually increase what I ate.
-On Saturday, I started transitioning from a clear diet to a low residue diet (Baby food, apple sauce, Jello, soup, toast, cereal/fiber/water).
-On Sunday, I started eating a bit more regular (1/4 cup all bran, spinach, sweet potatoes, lima beans, yogurt, cereal bar)
-On Monday, I had a ½ coffee cup of prune juice.
-Sunday night, I had some spasms but there were brief
-Four days after surgery (Monday), the medical center called and followed up.
-The nurse’s diagnosis: I was doing great
-As of Monday, I hadn’t had a BM yet.
-According to the nurse, if I didn’t have a BM by Thursday, that’s when I should worry.
I then spoke with my doctor and here’s what he said:
-Drainage - I have an open wound. There’s going to be drainage from it for about a month
-Incontincence - I probably won’t have good control for about a week
-I should keep the area clean
-Do the sitz bath
-After each, make sure I dab it dry so it doesn’t get an infection
-Swelling – Yes, there will be swelling
-Eating – I can eat just about anything. (Fish, chicken, etc).
-Yogurt – He said yogurt was good and I could eat 2 to 3 a day
-Bad food - Nuts, rice, spicy
-Spinach – he wasn’t too keen on me eating spinach. Because of the iron, he said it could constipate. I should probably stay away from it.
-Regarding blood, the nurse said that the time to become concerned is when you’re passing so much blood it’s filling the toilet bowl and stuff.
POST-OP ASSESSMENT (7/12)
-About a week after surgery, I visited the Doctor for a post-op assessment. On the morning before the visit, I finally passed a large amount of stool. This caused bleeding. To stop the bleeding, the surgeon did a procedure that I believe he called a “sulfur burn” and he put gauze in. The gauze will come out. I shouldn’t do a sitz bath that night (unless I have a BM).
-Regarding the fissure and hemorrhoid surgery, they look like they’re healing but it’s hard to tell with today’s wound.
-PAIN KILLERS –
He didn’t want to give me a new prescription. As I run out, I can start cutting back. Take two a day (or something) then I can start substituting regular Tylenol. DON’T TAKE TYLENOL AND HYDROCODON AT THE SAME TIME. As I cut back, I can alternate between the two. Don’t take more than one hydrocodon every 6 hours.
-Some people only need pain killers a couple of days. Others maybe a month
-For me, I should take Hydrocodon at night before I got to sleep, then 1 during the day.
-If I have a little pain, I can take a Tylenol. If I have a lot of pain, take a Hydrocodon
-Even now, I can try alternating between the two.
-BLOOD –
It’s okay if it’s dark blood that’s draining. I should be worried of it’s gushing or bright red. It’s going to drain for awhile. I should go to the emergency room if it’s gushing but other than that don’t worry. It’s just going to drain.
-BATHING –
-Over the weekend, I should avoid doing a sitz bath where I would be sitting. Instead, he suggested showering and dabbing the area. I can a resume sitz bath on Monday.
-DIET –
For now, don’t eat bran or eat it in smaller amounts.
For breakfast, I could eat eggs, bread , strawberries, raspberries, blueberries, etc.
For lunch, yogurt (It’s good for the GI—gastro intestinal), salad, fish (salmon okay), cantaloupe, green beans, lima beans, rice (just a little. It could constipate), stay away from spinach, stay away from lima beans (too high in fiber), stay away from anything that’s going to give me too much fiber, stay away from nuts and anything spicy
-Regarding a dietitian, he didn’t seem to think I needed one. If I wanted one, I could ask my primary care physician for one. (I eventually would and it would help immensely).
-Most patients take about six weeks to three months to heal
TWO WEEKS SINCE SURGERY
-After 2 weeks, 95% start getting back to normal and soreness starts to go away. I can also start eating things like chicken.
-I am off the Hydrocodon. I took a Tylenol this morning and I only need to take it as needed.
-For two weeks after surgery, I kept taking COLACE (the stool softener). After two weeks, I was instructed to stop.
-According to the nurse, I can take the COLACE up to a month but if I could start tapering off, that would be great
-She suggested I cut it back to one a day for the next week and see how that goes and slowly taper off. That would be fine.
-Multi-Vitamins – I shouldn’t start taking them yet. I should wait until after my next doctor visit and the Doc gives his okay
THREE WEEKS SINCE SURGERY
I had a follow up visit with my surgeon. He said the fissure and hemorrhoid looked okay. It will take a bit to heal completely. The results came back from the polyp biopsy. It was benign.
-RECOVERY TIME – He figures 2 to 3 weeks. Before I return to work, he will give me certification. I asked about any restrictions and he said that he isn’t going to give me any. I told him that I would need that in writing for my employer.
-When I return to work, I should sit on a cushion
-SITZ BATHS - I should continue them and I should make sure that I dab the area.
-INCONTINENCE - I don’t really have that any more. I will continue to have drainage and mucus for some time.
-GAUZE - I asked him if there was an issue with me putting gauze between my butt cheeks to deal with the drainage. He didn’t have a problem with that.
-EXERCISES – He wants me to do toning exercises each day. Basically, you tighten and contract the rectum for 10 seconds, then release. Do this 10 times each day.
-ERECTILE DYSFUNCTION / SEX - I shouldn’t have any issue with erectile dysfunction. I should hold off on any sex until I’m healed.
---ACTIVITIES –--
SITTING - I can sit but I may want to put a pillow beneath me.
STAIRS - I shouldn’t do a stair master but it’s okay for me to take stairs to get my mail.
DRIVING - He had some restrictions in regard to this. I told him that I wouldn’t do it just yet.
----DIET-----
Citrus - It’s okay to drink cranberry juice and eat oranges. Just stay away from spicy foods
MULTI-VITAMIN - It’s okay to take a multi-vitamin
-After 6 weeks to 2 months, the wound should heal. Again, the soreness will go away in about 2 weeks but it won’t be healed for 6 weeks to 2 months.
FIVE WEEKS AFTER SURGERY
I had trouble passing stool. My body kept wanting to go but nothing was coming out but small drops. This went on all day. Finally, at about 7:30pm, I had two small nuggets. Then, at 8:30pm, I had a large bowl movement. The next morning, I immediately had a medium sized bowel movement when I woke up, then an hour later, I passed one more normal sized stool.
I called the doctor and spoke with his nurse. I asked if these spasms were normal. She gave me her advice and she spoke with the doctor and said the following:
-They wanted to see me this week.
-It should be okay
-This is fairly normal post surgery and it’s fine.
-It may happen for a couple of weeks
-The muscles down there get tense. They don’t stretch and they spasm. It happens.
-She told me to drink a lot of water, take COLACE twice a day and take fiber.
-I told her that it seemed the stool was already kind of soft. She had thought that this wasn’t the case since I initially said that it was sort of harder.
-She said that if it seemed like it was already soft don’t take the COLACE.
-She said that you needed to take the COLACE for a bit for it to take effect. You can’t just take one and expect results.
-The sitz baths should help relax the muscles down there.
-She said that you should be doing about 30 grams of fiber a day.
-Three days after this call, I visited the doctor. I had a little flare up in the morning (My bowels wanted to pass but my sphincter wouldn’t open) Eventually, it did. Here’s what the doctor said:
-I am doing pretty well. The fissure and hemorrhoid look good.
-He checked the strength of my sphincter by sticking a pinky inside and having me squeeze. It was tight and the tone was good. I don’t have to do the exercises any more.
Regarding my other questions:
-Lumps on anus – What are they? / ETA for lumps to return to normal shape?
The lumps are hemorrhoids. They will eventually go down in size to nothing. This will probably happen in another month.
-Anus heal – How long? October or beyond?/
He felt in another six weeks it should be healed. Maybe 3 months total? Like he said, these things take some time.
Blood how long?
I’ll have a little blood for awhile. If it’s just a little on the tissue, that’s fine.
-Sphincter tightens/ stool won’t pass – normal? / How long? / Treatment?
This is normal. It may take a couple of weeks before it stops spasming
In a week or two, if it continues to spasm, I can apply the DILTIAZEM ointment that I have. Just put it on the outside. It relaxes the muscles.
Don’t take it if I don’t need it.
-Is this possibly the result of some IBD (Irritable Bowel Disease)? (Ulcerative colitis? Proctitis? Form first?)
-No. He didn’t think this was the result of any of these. They would’ve shown on the colonoscopy report that I gave him and they didn’t. I specifically asked about ulcerative colitis and proctitis. He said “No.”
-Should I continue taking stool softeners?
I can continue with these as long as I need them.
Activities –
-Walking is okay
-Driving is okay if there’s not pain
-Pushing a shopping cart I should avoid. It’s too heavy
-Laundry basket lifting – If it’s less than ten pounds, I can lift. Otherwise, no.
-Push ups – No. I shouldn’t do these.
-When can I go back to work? (Certification or extension?)
He said I could try it as long as there was no pain. I should use a cushion. I should alternate between standing working and sitting working, maybe every 20 minutes. I shouldn’t stand all the time or sit all the time either. He’s giving me no restrictions and she gave me a certification paper.
DIET
-He told me to avoid too much rice and bread. Eat plenty of fruits and veggies and water. He also told me I could drink prune juice. I told him that my bowels were fine. It was my anus that was the problem and I preferred to avoid prune juice all together.
-What can I do to avoid this in the future?
Fiber, fruits, veggies, and water. I can resume this as normal once healed.
METAMUCIL
Don’t take it now. I shouldn’t take it until I’m healed.
He wants to wait a month before seeing me again.
A MONTH LATER – NINE WEEKS AFTER SURGERY
It’s been one month. I had gone off of COLACE two days ago. A couple days prior to that, my stool had been diarrhea. Today, I was just passing nuggets in the morning. The doctor checked me out, stuck a finger up in there. He said that the stool that he felt was a little hard but not bad.
Here’s what he said:
-It’s healing nicely – but it’s still not healed. There’s no fissure or hemorrhoids
-There’s still an open wound that’s healing. The wound is almost closed.
-Scar tissue could tighten it but he wasn’t alarmed by my scar tissue
-Drainage & Blood - I will have drainage and blood until it closes. . Another month maybe two or more. Drainage comes from the wound.
-Hemorrhoid lumps – They may get smaller or they may stay that way. They won’t completely go away. They will only become a problem if later on I get constipated and push. At that time, I can have them removed.
-SCAR TISSUE - There will be scar tissue but he didn’t seem to think it would be an issue. Scar tissue will never go away. He didn’t say it was too tight or too wide. It was just a little tight. He felt it was healing nicely.
-He didn’t feel that it had healed too tight.
-Anus heal - It may not take until November. We’ll see.
-Sitz baths – At this point, they’re not promoting any healing. I can keep taking them for comfort if I’d like and to just soothe. Just be sure to dab dry avoid growth and infection.
-Difficulty passing stool - He didn’t seem to think it was the result of spasms. When he stuck his finger inside, he didn’t encounter any spasms.
-He seemed to think they were more diet related (Not IBS or spasms).
-STOOL SOFTENER - I could continue taking it but if it’s causing diarrhea, I should not take it
-Fiber supplement - He wanted me to start taking fiber. I asked if Citrucel was okay. He said “Yes” but I should take less than the dose they recommend (take half of what they say). It will bulk but bulk shouldn’t be an issue. I need to take two glasses of water with it and water should soften it. (If you don’t take it with lots of water, it could constipate)
-DIET – I’ve had such issues with hard stool and finding a diet that works. He said it’s really up to me to experiment and find a diet that works for me.
-Eat plenty of fruits and vegetables. I can eat chicken and fish, maybe even some meat once in awhile.
-Are there any positions that I should avoid?/ Will it be irritated if I sit or lay on my side? – He didn’t have any restrictions in regard to positions. Again, he said if I sit I can use a pillow. I told him it was more comfortable without one
-What can I do to avoid this in the future? - Avoid constipation
When I got home, I had a teaspoon of Citrucel and two pints of water. I immediately had a large BM.
ELEVEN WEEKS AFTER SURGERY
It was about a week and half since my last visit with the colorectal surgeon. I was still having trouble with hard stools and I had other questions. I paid another visit. Here’s what he said:
-My fissure is healed. However, my sphrincterotomy is still healing. It should be healed by October. Again, if you have hard stool, there will be pain normally. It looks more healed than last time. There could always be more bleeding with constipation though.
-HARD STOOLS –
-He suggested I visit the people who did my colonoscopy. They handled gastroenterology, liver disease and other aspects of digestive health.
-He thinks the hard stool is diet related. I need to drink more water.
He didn’t seem to think it was a sign of a bigger problem and that was a low chance.
-COLACE – I wondered how long I could take it without causing damage to myself. He said, “You can take it for a long period of time, three months or so. I had been having issues with diarrhea. When I stopped the COLACE, the diarrhea stopped.
Also, I had been having an issue where the skin around my right testicle began to droop while the testicle stayed ascended. This stopped as soon as I quit taking the COLACE. Odds where, it wasn’t the fault of COLACE. It was caused by an infection that was swelling my lymph nodes or something.
INFECTION
-I had some soreness and swelling on the left side of my inner buttocks, near my anus. I thought, it was just inflammation from the surgery. Before I left the office, I mentioned it. The doctor took a look and discovered it’s something more serious. It appears to be the beginning of an infection where the sphincterotomy incision is located. It has created an ANORECTAL ABCESS. It appears he caught it early. It’s still a bump.
-He says it’s a perirectal abcess
-There’s not much distance between the sphincterotomy wound and the abscess.
-There is a fistula tract. It’s superficial.
-I asked, “How did this happen?” He said the wound from the sphincterotomy became infected (despite the anti-biotics they gave me in my I-V at the time of surgery). When they made their incision, it was in the outer muscle (?) The one closest to the interior wall. He said that possibly the fissure closed too early and formed an abscess that became infected.
-It’s possible the infection could have come from a piece of stool getting clogged in a gland. He didn’t really know.
-He cut it some. He drained it a bit.
-They’re trying to take care of it so it won’t become something worse.
-He said that it looks like if I had to get surgery it would be pretty superficial.
-WHAT WILL IT LOOK LIKE IF IT WORSENS? – If it worsens, I should look for fever, chills, redness, swelling or excessive drainage
-GAUZE – He put gauze on it. I should keep the gauze on it until tonight or my first BM. (He even suggested I could take it off at 4pm then do a sitz bath)
ANTI-BIOTICS
**WARNING*** Over prescription of anti-biotics by doctors has lead to a rapid increase in the cases of C-Dif throughout the country. I know because it happened to me about a year after this in an unrelated incident. Anti-biotics kill the bad bacteria in your system. They also kill the good bacteria. When you stop taking the anti-biotics, there’s a chance the bad bacteria might start growing back faster than the good bacteria and out number it. Your body tries to flush the bad bacteria and you get constant diarrhea. If it isn’t treated, you could die. Again, if your doctor prescribes an anti-biotic, talk to them about the dangers of C-Dif and precautions that you should take to avoid it (like taking a pro-biotic that adds good bacteria to your system). I can’t stress this enough. The doctors are trying to help you but sometimes, they don’t think two steps ahead.
-C-DIF WARNING SIGNS – Diarrhea would be a sign. He said, I should eat plain yogurt to help combat this (If you have C-Dif, it will take a lot more than yogurt to combat it). He said it’s okay to have 2 to 5 BMs a day, as long as they’re not diarrhea.
-Now, getting back to my infection story…
-The doctor gave me two prescriptions for ANTI-BIOTICS (FLAGYL & CIPROFLOXACIN). I will start taking them. It may give me diarrhea.
-There is a 50/50 chance that the anti-biotics will work.
-I will see him again in two days. He’s going to do a procedure where he will make an incision and drain the abscess.
-On that day, I will need to have someone drive me and I will need to take the next week or two off.
-If this procedure and the anti-biotics don’t heal it, I will need to get surgery. For the surgery, they would stick a probe up my ass and a probe up the fistul and they would make a cut. Hopefully, they won’t have to do this. Hopefully, it will heal.
-When I had my initial surgery to fix the fissure, he had said there was a 5 to 10% chance that I would get an infection. I guess, I fell into that 5 to 10%.
-Sitz bath – I should keep taking them two times a day and after each BM.
-At work, I should sit on a pillow.
TWO DAYS LATER – ABCESS DRAIN
-The doctor performed an in-office procedure to drain the puss out of the ABCESS. It went very fast.
-He injected an anesthetic into it to numb it. Then, he cut an X over the area and drained it.
-He gave me a doctor’s excuse to take the next week off from work.
HIS INSTRUCTIONS POST ABCESS DRAIN PROCEDURE
-Keep the packing on it until the next morning or until after my first BM. (When it came time to remove the packing, I didn’t realize that the packing wasn’t just on the surface. The packing was actually a long strand of gauze that was packed down inside the wound. Pulling it out was like a magician doing a scarf trick. I had to pull a long strand of gauze out of the hole where my wound was. They hadn’t warned me of this. It wasn’t painful. It was just a little shocking to discover)
-Keep redressing the surface with gauze until I see him again in five days . I don’t need to tape it. I just need to keep the mess off of my clothes. I can just stick some gauze between my cheeks.
-At the first sign of pain, I can take an Extra-Strength Tylenol. He gave me a prescription for Hydrocodon if I need it. Again, I may not need it. I can take them with food and they won’t interfere with my anti-biotics. The Hydrocodon can constipate.
-I should continue to take sitz baths. According to the nurse, they are to help with the pain. I should dry the area afterward. Spread my cheeks and dab area dry.
-Don’t put creams or rubbing alcohol on it.
-For the next three days, don’t put much pressure on it. Lay on side that doesn’t have abscess.
There is hope - LIS and abscess
My diary - It took a year
Return to Anal Fissure Success Stories
- rockybalboa76
- Fibre Addict
- Posts: 24
- Topics: 2
- Joined: 12 Aug 2014, 14:36
- Has thanked: 0 time
- Been thanked: 14 times
- Gender:

Re: There is hope - LIS and abscess
FIVE DAYS AFTER ABCESS DRAIN/ ELEVEN WEEKS AFTER FISSURE SURGERY
-It looked like the ABCESS was healing.
-If it looked bad, it would be red and it would be swollen.
-Using a swab, he re-opened the wound so it would continue draining. They’ll do the same on my next visit. He’s trying to avoid the formation of a fistula.
-He put gauze down there again. I should take it out tonight. I asked him “When?” He said after twelve hours (8pm or 9pm-ish?) or my first BM if I’d like.
-I told him that I was having maybe one BM a day, maybe two and it was soft like diarrhea. He seemed to think this was fine and the result of the anti-biotics. If I was having diarrhea constantly it would be an issue
-Not only was the diarrhea coming out of my anus, I would see small drips of stool exiting the ABCESS wound as well. I asked him about this. He didn’t think this was too much of an issue infecting the abscess. Still, he told me to do sphincter clenching exercises 15 times a day.
-Regarding going back to work in a week, he felt that it was okay. I can sit. I should use a pillow. I can work and it’s okay to drive. I would need a note from the doctor saying I can work with no restrictions.
TWO WEEKS SINCE ABCESS DRAIN / THIRTEEN WEEKS SINCE FISSURE SURGERY
-I visited the doctor. He looked me over and said:
-MY ABSCESS WOUND – It appeared to be healing pretty well – but it’s too early to tell.
-I mentioned that after I have a BM, I can see stool draining out of the ABSCESS WOUND. He said that if that’s the case, I might need surgery. He would know within a month to six weeks.
-To help close the wound, he inserted and applied a silver nitrate stick. It cauterizes it and hopefully it will help with the closing.
-He put gauze down there. He said I can take it off later today.
-He said that if a fistula does develop it looks like it will be near the surface and it shouldn’t be too hard to heal
-DIFFERENCE BETWEEN AN ABSCESS AND A FISTULA – A fistula is chronic. He can’t tell at this point if I have a fistula or not.
-SKIN TAGS – Since my fissure surgery, there have been two, small fleshy lumps on the exterior of my anus. These are called SKIN TAGS. They are created during surgery when the skin expands and contracts. He told me not to worry about them at this point. They are normal. They can be shaved off with an office procedure if I’d like (although he eventually advised just leaving them)
-SITZ BATHS – Instead of doing it twice a day, I should just do it after each BM. It’s for comfort and to keep things clean. He didn’t feel it would help with the draining or swelling.
-ANTI-BIOTICS – Initially, he told me to stop taking them. I told him that I had some puss drain yesterday. Because of this, he prescribed that I continue taking the METRONIDAZOLE but not the CIPROFLOXACIN
-PROBIOTICS – I asked if I can take them while I’m on anti-biotics. He said that I probably could but I should ask the pharmacist. (I did. She said it was okay. Anti-biotics kills both the good and the bad bacteria. Probiotics help replenish the good bacteria.)
-ARE MOST PEOPLE HEALED BY NOW? – 5% aren’t.
-CONTACT THEM – If it starts causing pain, gets red or I have fever.
-MY NEXT VISIT – I will see him again in eight days. He will probably use another silver nitrate stick on me again.
By this point, I was battling a whole host of issues: the fissure healing, the abscess healing, my weight loss and my depression. I was second guessing my surgeon.
I went to my primary care physician and got referrals to another colorectal surgeon (in order to get a second opinion) and a dietician.
Regarding my healing: He said, if the puss is clear, it’s a sign it’s getting better and I probably don’t need the anti-biotics.
Also, the surgeon should’ve sent him a surgical report. He didn’t have it and I should tell the surgeon to send it.
-ANTI-BIOTICS – The stuff I’m on now (FLAGYL) is to help fight against C-Dif. When I come off of it, if I am having diarrhea, I should contact him immediately. That’s the C-Dif.
-When I come off of it, I should immediately start taking yogurt. Yogurt is the best for getting pro-biotics. Others are okay but yogurt is the best
-Sauerkraut – don’t take it within 1 hour of anti-biotics. It has milk in it according to him and could react with the anti-biotics
-VITAMIN C – I should be taking it to help with the healing the wounds
-TESTICLES – I told him that at some point, prior to having the abscess drained, I developed some soreness around my right testicle and some of the skin beneath the testicles would start to droop. He said that it sounded like the lymph nodes trying to fight the infection. They became swollen and that’s why it caused the issues in that area.
After I left my primary care physician, I went and visited the new colorectal surgeon that he recommended. He was terrible. It made me realize that my original surgeon was pretty good. So, I decided to stick with him, come Hell or high water.
My primary care doctor also recommended that I see a DIETICIAN. He gave me a referral and I should tell them to up my calories.
THREE WEEKS SINCE ABCESS DRAIN/ 14 WEEKS SINCE FISSURE SURGERY
I went back for a check up with my old colorectal surgeon.
STATUS OF ABSCESS/ INFECTION
-The sphincterotomy is still healing. There is a film over the wound. He did a finger exam and felt around in there. It may take another month to heal.
-FISSURE STATUS – Fissure is healed
-He still was unsure if I’d need further surgery or not.
-I asked if surgery for a fistula was as painful as for a fissure. He said there would be pain but it wouldn’t be fissure pain. (Still, there would be pain)
-ANTI-BIOTICS – I told him that I had a week’s supply. He told me to keep taking them for the next week. He says the METRONIDAZOLE that I’m taking helps with the healing of the fistula and it helps prevent C-Dif
-SLEEP POSITION – I worried that I needed to sleep in one position to help with the drainage. He said I can sleep and lay in any position that I like. It didn’t matter. I should sit on a pillow at work though.
-SITZ BATHS – He told me to do it twice a day after each BM. If I have a couple of BMs in the morning, maybe do it in the morning after my BMs, then once again at night when I get home.
-PAIN AFTER BM – He said this was normal. It’s normal to still have some drainage too.
WEIGHT LOSS ISSUE
While dealing with the fissure, I began eating less and less. I was afraid of ingesting something that might cause me pain when it came out the back end. As a result, I developed a mild eating disorder. My weight dropped to 133 pounds.
Since I was not getting good dietary advice from the surgeon or the doctor, I decided to take action myself and see a DIETITIAN/NUTRITIONIST. It was someone recommended by primary care physician.
The dietitian was at a hospital. When I arrived, they had me do a bunch of paperwork. The billing person claimed that since it was at a hospital it wasn’t considered a doctor’s visit. It would be considered an outpatient hospital visit. Instead of paying a regular co-pay of $20 or $30, I would be paying $300. She also asked if I wanted to pay it now. I told her to send the bill to my insurance company and they could haggle over it. Her attempt to get $300 immediately almost seemed like a con to me, like she was trying to get me to pay the full amount instead of having the insurance company talk them down and reduce the price. Beware of this hospital con. Don’t pay on the scene. Always have them send the bill to your insurance company.
Next, I visited with the dietitian. Here’s what she said:
-She would like me to add another 10 pounds. (Target weight around 144 lbs)
-It takes a long time to add weight. You can only add about 1 to 2 pounds a month.
It will take several months.
She seems to think the hard stools that caused the fissure happened because of:
-Too much protein drinks and protein powder
-Too much alcohol
-Too much coffee
-I think if you add all the rice I was eating to the picture, you see that it was all drying out the stool and making it too hard.
-Then, when I became stressed, it hardened the stool even more.
-She really stressed the point that the mind controls the whole body. If it’s stressed, it locks everything up down there. As a result, things would get hard.
-She said your intestine is lined with little gate keeper like things. When you get stressed, they lock up – and they make the stool very hard to pass. She seems to think this might have been happening when I had those spasm days.
-I need to learn to relax
-Stress can most definitely cause hard stool
PROTEIN DRINKS
-I told her about all the protein drinks and protein that I was taking around the time of the fissure (Powders can sometimes have 20g of protein)
-She said that protein dehydrates. Your kidneys don’t like it. They try to flush it out and with it, a lot of water goes with it, which then causes your stool to be hard.
-She wants me to stay below 100g of protein a day (120g would be the ultimate limit)
-Plus, I need to throw out all the protein powders and drinks. When exercising, I can get all the protein I need from foods. The powders will just mess me up.
NEW DIET
-To help me add weight, she suggested I add some of the following to my diet.
-She said I need high calories and high protein
-She just suggested that I take Vitamin A, Zinc and Vitamin C
-Spinach doesn’t constipate according to her. She seemed to think the doctor’s didn’t know what they were talking about.
-For the iron and stuff, she initially told me to eat more hamburger. She said eat meat balls, hamburger, ground beef
-Iron supplements can constipate but you don’t have to worry about iron in food constipating.
-Oat meal – it doesn’t constipate. Rarely
-Rice – I should limit it to ½ cup or less. Too much rice can constipate
-Pineapple is fine. She didn’t think it constipated at all
-I should add:
-Prune juice – I can drink 6 to 8oz before bed. This will make my morning stool soft.
I should either be eating 4 prunes or drink 6oz prune juice every day. This is high in iron and calories.
-Nutrigrain bars are fine. I can even try getting Quaker 100 calorie bars
Add between meals:
1 to 2 Tbsp of smooth peanut or almond butter
-peanut butter -- Peanut butter won’t constipate. This way, you don’t have to eat the hard peanuts
-You can put them on crackers
-2 Tbsp olive oil should be added to every meal
-Put margarine on crackers in the morning.
-1 whole avocado every day
-Silk – She thinks drinking it is great
-1 yogurt minimum each day
-Orange juice - Keep up drinking it. It has healing properties.
NO PROTEIN DRINKS!!!
-Too much protein, you pee it out. 120g is the limit
-No protein supplements
I don’t need to come back unless I’m having further issues.
So, I began adding these items to my diet. Within a week, I was having frequent diarrhea.
I called the dietician to see what the Hell went wrong:
-She didn’t really give me an answer. She just told me to basically cut back on the foods she suggested and ease into them.
-I checked with my primary care physician and asked, “Why do I have diarrhea?” He said, it’s because if you start taking too much fat too fast, your body rejects it. You have diarrhea. You have to ease into it. When you haven’t been eating a lot of fat and suddenly you start adding a lot of fat, your body tries to reject it. It flushes it out through diarrhea.
-I should gradually ease into adding the healthy fats so my body has time to adjust.
-For the next couple of days, cut out Prune Juice and Orange Juice
-The dietician said prunes can have no affect on people or it can cause the runs in others. You just have to play around with it to see how your body reacts
-Avocado is okay
-Peanut butter just do 1 teaspoon
-She told me to cut back on the Almond Butter. I told her I was going to cut it out completely
-I told her that I had chills on Sunday and Monday night – but I didn’t have a fever at the Doctor’s office. She said that fever can come and go. It does sound like I had a fever
-If I’m no better by the end of the week, I should set up an appointment to see her.
-After I got off the phone, I checked my temperature and it was 97.5 (Which is normal)
-I cut back and eased into the new diet. Eventually, the diarrhea stopped and I slowly began to add the necessary weight.
Also, during this time, I took action regarding my mental health, too. All of my health issues had created an incredible amount of stress, anxiety and depression. I realized, like with my weight issues, that neither my primary care doctor or surgeon was going to help me in that area. Luckily, my employer had an EAP (Employee Assistance Program). I called a number and I could set up eight free sessions with a therapist. I’m extremely glad that I did this because it helped me enormously to combat my mental stress and anxiety.
NOTES FROM MY MENTAL HEALTH THERAPY
-You need to do things to focus your mind elsewhere. Breathing deeply, repeating positive sayings, etc. really got me through it.
-Stress can inhibit healing. It tends to get localized in a particular body part and that body part gets worn out.
-I asked if my anxiety attacks might be the result of post-traumatic stress. She absolutely felt that was part of the issue.
-Breathing exercises are a good way to deal with anxiety
-I felt like I was forced to confront my own mortality. Everything seemed pointless.
-It felt like the child inside me had died. She told me that the child hasn’t died. It has gone into hiding. The adult had to take over because of the serious situation. Once I heal, the child will come out of hiding.
-You will heal. It’s not permanent.
FIND HARMONY
-I told her that I felt like a failure. She said that if anyone told me that I should point out that it’s DESTRUCTIVE THINKING
-There is positive and negative in everything. (Ex. It’s good I’m getting help – but it’s bad because it’s taking up time that I could use doing other things)
-I need to avoid focusing on the negative and restore the balance. Find the harmony.
CONTROLLED CONSCIOUSNESS
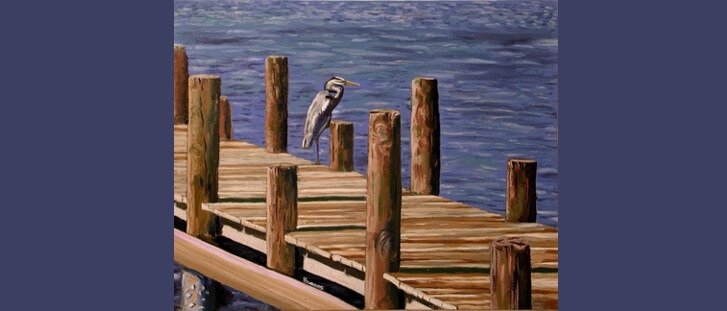
Whenever I feel that I’m focusing on the negative, I need to think of a positive event and replay it in my head from beginning to end. (Ex. I told her that I would imagine sitting on a beach or in my parent’s backyard)
ISOLATION
-I lived alone and it sounded like a majority of my issues came down to my isolation.
It makes me focus on myself and it creates a loop of negative thoughts. I become obsessed with things.
-Don’t isolate yourself. It’s important that you get involved with a group and don’t just connect with people on-line.
-You should meet with a group on a regular basis.
-Something that will be there week after week. Maybe a cooking class or a club of some type.
-She suggested volunteering at a nursing home and having a surrogate parent.
-DETACHMENT – When I’m in a group and I feel detached, this is me trying to protect myself. It’s part of the post traumatic stress and it will eventually correct itself
IF YOU FEEL SUICIDAL
-People feel suicidal because they feel overwhelmed
-If you feel suicidal, you should call 911
-Tell them that you’re suicidal and you need assistance.
-They will put you in contact with their PET Squad (Psychological Emergency Team)
-They will send an ambulance and take you to a psychiatric center and monitor you for 72 hours
IF YOU START TO FEEL BAD AGAIN:
-It’s important to recognize the bad thoughts and take action to steer your mind in a good direction as quickly as possible.
-When you have a bad thought, stop, breathe deeply and remind yourself there’s a lot of things in your life that are working
-Write, shoot and direct an image in your head where the future event that you’re worried about works out (I can have it right along with a script where it doesn’t work out but I need to also come up with one where it does work out)
-It is better to think of a positive memory, playing it from beginning to end or think of a desired outcome, playing it from beginning to end
ANTI-ANXIETY MEDICATION
-My therapist recommended visiting my primary care physician and asking for some anti-anxiety medication. I should tell him that I’m stressed and my therapist recommends I take something for my stress during this challenging time
-When I did visit my primary care physician, he agreed and put me on CITALOPRAM (aka CELEXA) – Anti-anxiety medication. It ended up making a huge difference and I wished I had been on it earlier.
-I told therapist that some of the relaxation techniques that I had been doing weren’t working any more. She said that I’ve been traumatized. Of course some of my relaxation techniques won’t work any more because I’m exhausted. I should try some new ones.
-She said that I will get better. I shouldn’t think I’m foolish because I had hope for things that didn’t happen. That’s a self esteem thing.
-I need to build my self esteem and confidence. If someone tries to knock me, I need to stand my ground.
-Negative comments only get under your skin if you don’t have confidence in yourself.
-If I have anxiety about something, it’s because my gut detects an issue. If this happens, I should follow this routine:
-DETECT PROBLEM – DO SOMETHING TO CORRECT IT
-The quicker I can get to “do something to correct it” the less I’ll worry. Plus, just knowing that I’m going to do something to correct it will help reduce the worry.
-I NEED TO BE A FRIEND TO MYSELF – I am too hard on myself. I need to be a friend to myself and treat myself like a friend, instead of being harshly critical all the time.
-I should publicly celebrate my successes
-Although some people go the other way and celebrate themselves too much, I have gone the other way and have made myself invisible. I need to celebrate myself more.
-DOWN TIME – I need to schedule some down time each day so that I relax. It’s not good to be constantly in a hurry. I should set aside time each day to do this and read or watch TV or nap. This is part of being a friend to myself.
WHEN PEOPLE ASK ABOUT MY CONDITION
She said that it’s not appropriate to go into the details. I can just tell them that I’m healing and move on.
END OF THERAPY NOTES
SIX WEEKS SINCE ABCESS DRAIN/ 17 WEEKS SINCE FISSURE SURGERY
STATUS OF ABSCESS/ INFECTION
-I went for a follow up with my surgeon. He probed me with a finger and had me squeeze. He said my strength back there was good.
-SPHINCTEROTOMY WOUND – It’s still healing. There’s a divot there which he says is a good thing. It looks like it’s healing over. He feels it will take 3 to 6 months to see if it heals completely.
-INFECTION – He can’t tell yet if it’s over or not. It doesn’t look bad.
He was happy that he felt a divot there – but he was concerned that when he pushed on the abscess wound, puss came out the other end (rectum). I should continue to watch out for chills, fever, pain, redness, swelling.
-SURGERY – There’s still no verdict on whether I’ll need surgery or not. There’s a 60/40 chance (60 I won’t/ 40 I will) Even if there is a surgery, he says it looks like it will be minor because it looks superficial
-SITZ BATHS – I should just take them after my BMs. I don’t have to take them before I go to bed. They’re just for cleansing mainly. Some soothing. They really don’t help with the healing
-WORKOUTS – I can do push ups. If I work out and I get sweaty, I should make sure that I rinse the area down there afterward.
A week after this, I made a return visit to my primary care physician because of three issues:
STRESS
-My therapist suggested I talk to him about prescribing something to ease my anxiety and stress. He thought it was a good idea. He said that stress and anxiety can definitely lead to a fissure because the constant tightening down there can wear on the area and wear it down. That’s why most of the things to fix a fissure are about easing the tightening down there.
The medicine he prescribes
-He prescribed the anti-anxiety medication CITALOPRAM (aka CELEXA).
-It won’t constipate and won’t stop the healing (In the old days, the medicine would constipate but not any more)
-I should start taking the medicine. It won’t kick in right away. It will probably take a week. I should take one in the morning. They will give me an initial supply of 30 and see how that goes.
-(NOTE: In hindsight, I wish that I had thought to ask about an anti-anxiety medication earlier. Celexa really helped reduce my stress which then helped reduce the hard stool issue that I was having, too. I would continue to take it until the abscess was completely healed.)
MY TONGUE FUZZ
-About a week and a half ago, it started feeling lumpy and the center of it turned black and a fuzz began growing on top. It’s a little better. He checked it out. He says it’s a yeast infection (aka thrush) that was brought on by the anti-biotics that I was taking. It’s a common occurrence. He asked if I was eating yogurt. I told him about all the yogurt that I was eating. Apparently, it wasn’t enough. He’s going to prescribe some stuff.
-He prescribed MYCOSTATIN (aka NYSTATIN)
-It’s a liquid and it’s okay to take it at the same time as the anti-anxiety stuff
-It comes in a bottle. They give you a little syringe like thing that you fill up with about 3cc of Mycostatin (aka Nystatin), then you inject it into your mouth on top of your tongue. You then swish it around for a minute, then swallow (They usually say 3 minutes but nobody can do it that long)
HARD STOOL
-I’ve been getting some harder stool in the morning.
-I’ve been also getting some mucus with it
-He immediately said it was the result of IBS (irritable bowel syndrome)
-Chronic stress can cause mucus and it can weaken the skin down around the anus.
-If I keep having hard stool, I should take MERALEX (a stool softener). Don’t take the amount they recommend. Just add a ½ teaspoon to my prune juice if I need it. It will pull water into my stool. I should take it in small doses. (A quarter cap?) It will probably take 3 to 4 days to work
-IBS goes back and forth between constipation and diarrhea
NINE WEEKS SINCE ABCESS DRAIN/ 20 WEEKS SINCE FISSURE SURGERY
I went back for a follow up with my colorectal surgeon. Here’s what he said:
-He examined me and probed me with his finger. He had me squeeze and said my strength back there was real good.
-It looked like it’s healing. It doesn’t look like there’s an infection.
-Feeling around where the abscess was, he feels something. He thinks it might be scar tissue or possibly a fistula. (If it turns out to be a fistula, I will need surgery)
-I don’t have any symptoms but I should keep watching.
-He didn’t see any drainage. If I should have drainage, I should give him a call and have a return visit. The last time I was there, he saw clear drainage and that’s a sign that it’s healing.
-I might have a little blood back there after he probed me. This is nothing to worry about. It’s just from the probing. (He examined me with his finger, then with a probe)
-It might take 3 to 6 months to see what it will do. The further out you get from it without any trouble, the better it is.
-I told him about the two medicines that primary care physician put me on. (Nystatin and Citalopram)
-SITZ BATHS – I should continue what I’m doing. It seems to be working. It’s mainly for comfort. When drying off afterward, I should spread my cheeks and clean up in there but I don’t need to go up inside.
-If I have a BM at work, I should just make sure I clean the area. I should take my own TOILET PAPER to work because it will be softer. Usually, the toilet paper provided at an office is cheap, rough and scratchy. Using your own toilet paper will save a lot of discomfort if I have to wipe the area a lot.
-There’s nothing else I can do to help it heal. Just keep doing what I’m doing.
-SPHINCTEROTOMY WOUND – It’s still healing. It’s a divet that’s filling.
-Again, the further out from this, the better my chances. It looks good, like it’s healing but I still have to be watchful.
-He wanted to see me in a month. I told him I would be out of town. He said that’s fine (I only need to come back right away if I see drainage)
-I explained what my stool was like (solid but soft enough to coil up). He seemed to think this was fine.
I went back to see my primary care physician to check up on the following:
MY TONGUE
-It still has a black, fuzzy patch. He called it the black hairy tongue.
-He said that the Infectious Disease Center says not to treat it. It’s an imbalance and your body will take care of it.
-He tried to knock it out with the Nystatin. It didn’t work. He told me to stop taking the Nystatin
-He’s going to give me an anti-fungal pill (LAMASIL 250mg)
-I should take it for 30 days then stop
-Hopefully, it should knock it out
ANXIETY
-He wants me to continue taking the anti-anxiety pill until after my fissure stuff is healed.
-He’s giving me a 90 days supply
-The dosage that I’m taking is low enough that I won’t have to taper off when it comes time to stop the medication
-I can take both the anti-fungal and the anti-anxiety in the morning together
-I can take them with food.
-When I run out of the anti-anxiety, I should tell the pharmacy to call my primary care physician and get authorization for a refill.
14 WEEKS SINCE ABCESS DRAIN/ 25 WEEKS SINCE FISSURE SURGERY
I went back for a follow up with my colorectal surgeon. Here’s what he said:
-It looks good. The sphincterotomy is covered. The infection is healed
-He doesn’t feel a tract. There’s no fistula
-You can still get an infection
-Everyone can. It’s like getting a zit. A gland can get clogged like a zit
-There’s just not one at this point
-He thinks the infection occurred after the surgery, not before
-I don’t have to continue the sitz baths. If I do continue, it would just be for comfort.
-After each BM, I should wipe, rinse and dry. I can part the cheeks and dab a little.
-Incontinence – He felt down there and said that I have good strength. It shouldn’t be an issue.
-If I like, I can do sphincter strengthening exercises. I clench the sphincter for 10 to 15 seconds, then release. Do this 10 times in a row each day for however many days I’d likes
-Sweat – If I sweat down there, I should dab it dry. Everyone should. If I can’t get to it for 8 hours, it won’t be a crime. Just get to it as soon as I can.
-After a shower, everyone should make sure they dry down there.
NINE WEEKS LATER…
I went back to see my primary care physician. My anxiety medication (CITALOPRAM 20mg) was about to run out. I had 8 pills left. He suggested I do the following:
-I should stop cold turkey.
-I may feel dizzy for 2 weeks
-It may take a week or so for the medication to get out of my system
-It will take 4 to 6 weeks to see what the psychological change is like
-This will occur about a month and a half from now.
-I should see how it feels and make a judgement
-If I decide to continue going without it, I should let them know that I’m going forward without it
-If the anxiety comes back and I feel that I should go back on it, I can go back on it.
-I would stay on it for a year, then get off it after a year
-It takes about a year of taking the drug for it to change the chemistry of the brain. Once it’s done its’ thing, hopefully, I wouldn’t need it any more and it will have changed my anxiety for the better
-He kept asking me if I thought I had a lot of anxiety before the fissure incident. Without hesitation, I said, “Yes.” He said a lot of people with anxiety get fissures.
-I should call them in a few weeks and let them know if I’m staying off of it or getting back on it.
-At this point, I still have 8 pills left. If the dizzy-ness gets too bad while I’m withdrawing, I can start taking the pills again and slowly ween myself off
-SLEEP – He seemed to think that the CITALOPRAM wouldn’t make me drowsy. It would make me more relaxed and less anxious. This would probably make me less likely to wake up when I should be sleeping
-If I start taking it again, he suggest to take it before bed time and see if I’m still falling asleep again in the morning.
-I can take the pill with prune juice.
-SEX DRIVE – Yes, CITALOPRAM affects sex drive. In fact, they prescribe the same medication for pre-mature ejaculation. If I decide I want an anti-anxiety medication again, they can put me on something that won’t affect the sex drive.
27 WEEKS SINCE ABCESS DRAIN/ 38 WEEKS SINCE FISSURE SURGERY (And almost a year since the fissure started developing.)
I went back for a follow up. He asked me: Am I bleeding? Do I have puss? Am I sore? Chills? Fever? I answered “No” to all of these.
He examined me and said:
-It is healed and the infection is gone
-This maybe the last time I have to visit him
-I told him I was off the anti-anxiety medication and I’m not doing sitz bathes since the last visit
-MUSCLE STRENGTH – He asked me to push. I told him I didn’t do that any more. He said I didn’t have to and he examined any way. He probed me with his finger and told me to squeeze. He said I had good muscle strength. He asked if I had trouble controlling BMs. I told him “No.” I can hold it until I get to the bathroom. I said that every once in awhile I might slip a little gas. He said that it’s normal and probably a result of the surgery.
I told him that sometimes it takes forever to wipe the area clean. Again, he said that it was probably a result of the surgery and normal. He mentioned that I could always have surgery to get rid of the skin tags on the exterior of my anus but he seemed to not want to advise that. I should just live with it.
If I’m worried about the strength down there, I can do the sphincter strengthening exercises. You squeeze and hold for about 10 to 15 seconds and release. Do this about 10 times a night.
-SWEAT – If I sweat after a work out, I should definitely shower and dab the area. If I climb stairs or sweat during the night, I don’t have to freak out. Just clean the area later
-EXERCISE & SQUATS – I told him that I had experienced some pain down there after doing squats while trying to exercise. He said I might have created a small hemorrhoid down there when I did it. Lifting heavy things can pop a hemorrhoid.
It’s natural for your body to create hemorrhoids. It creates them to cushion the BM that come through. The hemorrhoid can go away or they can stay and become trouble. If I get a little red, sore and irritated down there, I can apply some DESATIN (I am unsure of the spelling) People use it to help their kids with diaper rash. I should only use it if I feel I need it. Since there’s no open wound down there, it shouldn’t be a problem.
There are no restrictions on the exercises I can do.
-**NOTE** Later, I came to realize that the scar tissue healed down there and became rigid. When I did certain exercises like sit ups, it would strain the scar tissue and make it sore. So, I stopped doing certain kinds of exercises, adjusted my work out and things were fine.
-FOOD – Not too much RICE, BREAD or NUTS. They can constipate. SPICY FOOD isn’t the best either.
COFFEE is okay. In fact, it can act as a stimulant.
I asked him what I should do to avoid getting a fissure in the future. He said eat plenty of fruits, vegetables, bran. Drink plenty of water.
I asked about things to watch out for and he pretty much told me the same stuff that I already know.
-The nurse said I finally graduated
-I thanked them both for their help and left.
-They said if I have any other issues, I know where I can find them.
A YEAR SINCE MY FIRST DOCTOR VISIT REGARDING THE FISSURE.
31 WEEKS SINCE ABCESS DRAIN
42 WEEKS SINCE FISSURE SURGERY
I’ve been doing really well. No issues. On Monday, 4/29, I worked out with some weights. The next morning, when I had my BM, I noticed some blood on the stool and blood on the tissue. I thought that it might be nothing but I thought I should get it checked out. That night, I had another BM. It seemed to have a few faint traces of blood but nothing much. I did notice that I had a large hemorrhoid that night. It went away the next morning. The BMs that I had since then contain no blood and seemed fine.
My colorectal surgeon checked me out. He felt around, put a scope in and said the following:
-It’s not the fissure or the surgery. That looks fine and it’s not an infection
-There did seem to be a small hemorrhoid but nothing to be too concerned with
-He gave me a prescription for a suppository (HYDROCORTISONE SUPPOSITORY). I should only take it if I’m bleeding again. It contains steroids and I shouldn’t take it forever. It will reduce the swelling of the hemorrhoid.
-Alternating between standing and sitting at work shouldn’t affect the hemorrhoid (In fact, that activity is for other health benefits, fights obesity)
-Exercise – I should avoid my workout for awhile. He thought that any kind of exercise (push ups, weights etc) would probably affect it. It should just hold off for awhile, maybe use small weights. There’s no rhyme or reason why exercise sometimes doesn’t cause hemorrhoids and other times it does.
-He wanted to see me again in 2 months. If everything is okay at that time, I can cancel the appointment.
-After that visit, I didn’t have any issues. I ended up canceling the next appointment because I didn’t need it.
-Once in a while, I would get a little blood with a BM. It wasn’t much but it did alarm me. When I saw this, I would put on a latex glove, lay on my side and insert one of the HYDROCORTISONE SUPPOSITORIES. With the tip of my finger, I would hold it for a few moments. The suppositories melt when in contact with body temperature and they have a tendency to shoot right back out if you don’t hold it there for a few seconds. I would lay on my side for maybe 5 to 10 minutes and let the suppository melt, then I’d get up, dab away the excess liquid and things would be fine.
-The next day, I wouldn’t have any blood.
-As time went on, I took better care of myself.
-I drank plenty of water
-I ate plenty of fiber
-I cut out alcohol and coffee
-Before I went to bed, I would drink a half cup of prune juice, to make passing stool the next morning easier.
-When I woke up in the morning, I would take a large glass of water and drink down a probiotic pill (CULTURELLE). It seemed to help with my digestion and it seemed to me that I stopped having issues with hard stool.
-After awhile, I suspected that part of my issue with hard stool was a bacterial imbalance in my digestive tract. Because of years of abuse and family history, I didn’t have enough good bacteria in my digestive system. That’s why I started taking the probiotic and it seemed to help
-Other good sources of probiotics are yogurt, Kefir (it’s a drink) or sauerkraut. (Although with the Kefir, I did seem to have a few issues. I suspect it might be because of some lactose intolerance. I cut it out and I was fine).
IN REVIEW
-WARNING SIGNS – A warning sign of a potential fissure would be pain down there. That’s when I should see him. (Or trouble going to the bathroom)
-SUPPOSITORIES – HYDROCORTISONE – You need a prescription to get them. You can get an over the counter cream and apply it to the hemorrhoid if you’d like. It’s not as powerful as the suppository but it might do the trick. The purpose of the suppositories is the shrink the inflammation.
-He said that everybody has hemorrhoids. Only some get so bad that they become chronic. You can get them from straining. Weightlifters get them because they are straining so hard. As long as I don’t get into heavy, heavy weightlifting, I should be fine. Just be sure to rinse down there after working out.
-MIRA-LAX – It’s a stool softener. He doesn’t recommend taking it forever. Take only as needed. One long term effect of taking it too long would be that it stains the inside of the colon.
-CITRUCIL – It’s a fiber supplement. It’s fine to take this a long time. It’s just fiber.
-SKIN TAGS – He called them hemorrhoids. If they become an issue, I can have them removed but he doesn’t recommend it if I don’t have to. He can see that they might cause some issues when wiping.
-It looked like the ABCESS was healing.
-If it looked bad, it would be red and it would be swollen.
-Using a swab, he re-opened the wound so it would continue draining. They’ll do the same on my next visit. He’s trying to avoid the formation of a fistula.
-He put gauze down there again. I should take it out tonight. I asked him “When?” He said after twelve hours (8pm or 9pm-ish?) or my first BM if I’d like.
-I told him that I was having maybe one BM a day, maybe two and it was soft like diarrhea. He seemed to think this was fine and the result of the anti-biotics. If I was having diarrhea constantly it would be an issue
-Not only was the diarrhea coming out of my anus, I would see small drips of stool exiting the ABCESS wound as well. I asked him about this. He didn’t think this was too much of an issue infecting the abscess. Still, he told me to do sphincter clenching exercises 15 times a day.
-Regarding going back to work in a week, he felt that it was okay. I can sit. I should use a pillow. I can work and it’s okay to drive. I would need a note from the doctor saying I can work with no restrictions.
TWO WEEKS SINCE ABCESS DRAIN / THIRTEEN WEEKS SINCE FISSURE SURGERY
-I visited the doctor. He looked me over and said:
-MY ABSCESS WOUND – It appeared to be healing pretty well – but it’s too early to tell.
-I mentioned that after I have a BM, I can see stool draining out of the ABSCESS WOUND. He said that if that’s the case, I might need surgery. He would know within a month to six weeks.
-To help close the wound, he inserted and applied a silver nitrate stick. It cauterizes it and hopefully it will help with the closing.
-He put gauze down there. He said I can take it off later today.
-He said that if a fistula does develop it looks like it will be near the surface and it shouldn’t be too hard to heal
-DIFFERENCE BETWEEN AN ABSCESS AND A FISTULA – A fistula is chronic. He can’t tell at this point if I have a fistula or not.
-SKIN TAGS – Since my fissure surgery, there have been two, small fleshy lumps on the exterior of my anus. These are called SKIN TAGS. They are created during surgery when the skin expands and contracts. He told me not to worry about them at this point. They are normal. They can be shaved off with an office procedure if I’d like (although he eventually advised just leaving them)
-SITZ BATHS – Instead of doing it twice a day, I should just do it after each BM. It’s for comfort and to keep things clean. He didn’t feel it would help with the draining or swelling.
-ANTI-BIOTICS – Initially, he told me to stop taking them. I told him that I had some puss drain yesterday. Because of this, he prescribed that I continue taking the METRONIDAZOLE but not the CIPROFLOXACIN
-PROBIOTICS – I asked if I can take them while I’m on anti-biotics. He said that I probably could but I should ask the pharmacist. (I did. She said it was okay. Anti-biotics kills both the good and the bad bacteria. Probiotics help replenish the good bacteria.)
-ARE MOST PEOPLE HEALED BY NOW? – 5% aren’t.
-CONTACT THEM – If it starts causing pain, gets red or I have fever.
-MY NEXT VISIT – I will see him again in eight days. He will probably use another silver nitrate stick on me again.
By this point, I was battling a whole host of issues: the fissure healing, the abscess healing, my weight loss and my depression. I was second guessing my surgeon.
I went to my primary care physician and got referrals to another colorectal surgeon (in order to get a second opinion) and a dietician.
Regarding my healing: He said, if the puss is clear, it’s a sign it’s getting better and I probably don’t need the anti-biotics.
Also, the surgeon should’ve sent him a surgical report. He didn’t have it and I should tell the surgeon to send it.
-ANTI-BIOTICS – The stuff I’m on now (FLAGYL) is to help fight against C-Dif. When I come off of it, if I am having diarrhea, I should contact him immediately. That’s the C-Dif.
-When I come off of it, I should immediately start taking yogurt. Yogurt is the best for getting pro-biotics. Others are okay but yogurt is the best
-Sauerkraut – don’t take it within 1 hour of anti-biotics. It has milk in it according to him and could react with the anti-biotics
-VITAMIN C – I should be taking it to help with the healing the wounds
-TESTICLES – I told him that at some point, prior to having the abscess drained, I developed some soreness around my right testicle and some of the skin beneath the testicles would start to droop. He said that it sounded like the lymph nodes trying to fight the infection. They became swollen and that’s why it caused the issues in that area.
After I left my primary care physician, I went and visited the new colorectal surgeon that he recommended. He was terrible. It made me realize that my original surgeon was pretty good. So, I decided to stick with him, come Hell or high water.
My primary care doctor also recommended that I see a DIETICIAN. He gave me a referral and I should tell them to up my calories.
THREE WEEKS SINCE ABCESS DRAIN/ 14 WEEKS SINCE FISSURE SURGERY
I went back for a check up with my old colorectal surgeon.
STATUS OF ABSCESS/ INFECTION
-The sphincterotomy is still healing. There is a film over the wound. He did a finger exam and felt around in there. It may take another month to heal.
-FISSURE STATUS – Fissure is healed
-He still was unsure if I’d need further surgery or not.
-I asked if surgery for a fistula was as painful as for a fissure. He said there would be pain but it wouldn’t be fissure pain. (Still, there would be pain)
-ANTI-BIOTICS – I told him that I had a week’s supply. He told me to keep taking them for the next week. He says the METRONIDAZOLE that I’m taking helps with the healing of the fistula and it helps prevent C-Dif
-SLEEP POSITION – I worried that I needed to sleep in one position to help with the drainage. He said I can sleep and lay in any position that I like. It didn’t matter. I should sit on a pillow at work though.
-SITZ BATHS – He told me to do it twice a day after each BM. If I have a couple of BMs in the morning, maybe do it in the morning after my BMs, then once again at night when I get home.
-PAIN AFTER BM – He said this was normal. It’s normal to still have some drainage too.
WEIGHT LOSS ISSUE
While dealing with the fissure, I began eating less and less. I was afraid of ingesting something that might cause me pain when it came out the back end. As a result, I developed a mild eating disorder. My weight dropped to 133 pounds.
Since I was not getting good dietary advice from the surgeon or the doctor, I decided to take action myself and see a DIETITIAN/NUTRITIONIST. It was someone recommended by primary care physician.
The dietitian was at a hospital. When I arrived, they had me do a bunch of paperwork. The billing person claimed that since it was at a hospital it wasn’t considered a doctor’s visit. It would be considered an outpatient hospital visit. Instead of paying a regular co-pay of $20 or $30, I would be paying $300. She also asked if I wanted to pay it now. I told her to send the bill to my insurance company and they could haggle over it. Her attempt to get $300 immediately almost seemed like a con to me, like she was trying to get me to pay the full amount instead of having the insurance company talk them down and reduce the price. Beware of this hospital con. Don’t pay on the scene. Always have them send the bill to your insurance company.
Next, I visited with the dietitian. Here’s what she said:
-She would like me to add another 10 pounds. (Target weight around 144 lbs)
-It takes a long time to add weight. You can only add about 1 to 2 pounds a month.
It will take several months.
She seems to think the hard stools that caused the fissure happened because of:
-Too much protein drinks and protein powder
-Too much alcohol
-Too much coffee
-I think if you add all the rice I was eating to the picture, you see that it was all drying out the stool and making it too hard.
-Then, when I became stressed, it hardened the stool even more.
-She really stressed the point that the mind controls the whole body. If it’s stressed, it locks everything up down there. As a result, things would get hard.
-She said your intestine is lined with little gate keeper like things. When you get stressed, they lock up – and they make the stool very hard to pass. She seems to think this might have been happening when I had those spasm days.
-I need to learn to relax
-Stress can most definitely cause hard stool
PROTEIN DRINKS
-I told her about all the protein drinks and protein that I was taking around the time of the fissure (Powders can sometimes have 20g of protein)
-She said that protein dehydrates. Your kidneys don’t like it. They try to flush it out and with it, a lot of water goes with it, which then causes your stool to be hard.
-She wants me to stay below 100g of protein a day (120g would be the ultimate limit)
-Plus, I need to throw out all the protein powders and drinks. When exercising, I can get all the protein I need from foods. The powders will just mess me up.
NEW DIET
-To help me add weight, she suggested I add some of the following to my diet.
-She said I need high calories and high protein
-She just suggested that I take Vitamin A, Zinc and Vitamin C
-Spinach doesn’t constipate according to her. She seemed to think the doctor’s didn’t know what they were talking about.
-For the iron and stuff, she initially told me to eat more hamburger. She said eat meat balls, hamburger, ground beef
-Iron supplements can constipate but you don’t have to worry about iron in food constipating.
-Oat meal – it doesn’t constipate. Rarely
-Rice – I should limit it to ½ cup or less. Too much rice can constipate
-Pineapple is fine. She didn’t think it constipated at all
-I should add:
-Prune juice – I can drink 6 to 8oz before bed. This will make my morning stool soft.
I should either be eating 4 prunes or drink 6oz prune juice every day. This is high in iron and calories.
-Nutrigrain bars are fine. I can even try getting Quaker 100 calorie bars
Add between meals:
1 to 2 Tbsp of smooth peanut or almond butter
-peanut butter -- Peanut butter won’t constipate. This way, you don’t have to eat the hard peanuts
-You can put them on crackers
-2 Tbsp olive oil should be added to every meal
-Put margarine on crackers in the morning.
-1 whole avocado every day
-Silk – She thinks drinking it is great
-1 yogurt minimum each day
-Orange juice - Keep up drinking it. It has healing properties.
NO PROTEIN DRINKS!!!
-Too much protein, you pee it out. 120g is the limit
-No protein supplements
I don’t need to come back unless I’m having further issues.
So, I began adding these items to my diet. Within a week, I was having frequent diarrhea.
I called the dietician to see what the Hell went wrong:
-She didn’t really give me an answer. She just told me to basically cut back on the foods she suggested and ease into them.
-I checked with my primary care physician and asked, “Why do I have diarrhea?” He said, it’s because if you start taking too much fat too fast, your body rejects it. You have diarrhea. You have to ease into it. When you haven’t been eating a lot of fat and suddenly you start adding a lot of fat, your body tries to reject it. It flushes it out through diarrhea.
-I should gradually ease into adding the healthy fats so my body has time to adjust.
-For the next couple of days, cut out Prune Juice and Orange Juice
-The dietician said prunes can have no affect on people or it can cause the runs in others. You just have to play around with it to see how your body reacts
-Avocado is okay
-Peanut butter just do 1 teaspoon
-She told me to cut back on the Almond Butter. I told her I was going to cut it out completely
-I told her that I had chills on Sunday and Monday night – but I didn’t have a fever at the Doctor’s office. She said that fever can come and go. It does sound like I had a fever
-If I’m no better by the end of the week, I should set up an appointment to see her.
-After I got off the phone, I checked my temperature and it was 97.5 (Which is normal)
-I cut back and eased into the new diet. Eventually, the diarrhea stopped and I slowly began to add the necessary weight.
Also, during this time, I took action regarding my mental health, too. All of my health issues had created an incredible amount of stress, anxiety and depression. I realized, like with my weight issues, that neither my primary care doctor or surgeon was going to help me in that area. Luckily, my employer had an EAP (Employee Assistance Program). I called a number and I could set up eight free sessions with a therapist. I’m extremely glad that I did this because it helped me enormously to combat my mental stress and anxiety.
NOTES FROM MY MENTAL HEALTH THERAPY
-You need to do things to focus your mind elsewhere. Breathing deeply, repeating positive sayings, etc. really got me through it.
-Stress can inhibit healing. It tends to get localized in a particular body part and that body part gets worn out.
-I asked if my anxiety attacks might be the result of post-traumatic stress. She absolutely felt that was part of the issue.
-Breathing exercises are a good way to deal with anxiety
-I felt like I was forced to confront my own mortality. Everything seemed pointless.
-It felt like the child inside me had died. She told me that the child hasn’t died. It has gone into hiding. The adult had to take over because of the serious situation. Once I heal, the child will come out of hiding.
-You will heal. It’s not permanent.
FIND HARMONY
-I told her that I felt like a failure. She said that if anyone told me that I should point out that it’s DESTRUCTIVE THINKING
-There is positive and negative in everything. (Ex. It’s good I’m getting help – but it’s bad because it’s taking up time that I could use doing other things)
-I need to avoid focusing on the negative and restore the balance. Find the harmony.
CONTROLLED CONSCIOUSNESS
Whenever I feel that I’m focusing on the negative, I need to think of a positive event and replay it in my head from beginning to end. (Ex. I told her that I would imagine sitting on a beach or in my parent’s backyard)
ISOLATION
-I lived alone and it sounded like a majority of my issues came down to my isolation.
It makes me focus on myself and it creates a loop of negative thoughts. I become obsessed with things.
-Don’t isolate yourself. It’s important that you get involved with a group and don’t just connect with people on-line.
-You should meet with a group on a regular basis.
-Something that will be there week after week. Maybe a cooking class or a club of some type.
-She suggested volunteering at a nursing home and having a surrogate parent.
-DETACHMENT – When I’m in a group and I feel detached, this is me trying to protect myself. It’s part of the post traumatic stress and it will eventually correct itself
IF YOU FEEL SUICIDAL
-People feel suicidal because they feel overwhelmed
-If you feel suicidal, you should call 911
-Tell them that you’re suicidal and you need assistance.
-They will put you in contact with their PET Squad (Psychological Emergency Team)
-They will send an ambulance and take you to a psychiatric center and monitor you for 72 hours
IF YOU START TO FEEL BAD AGAIN:
-It’s important to recognize the bad thoughts and take action to steer your mind in a good direction as quickly as possible.
-When you have a bad thought, stop, breathe deeply and remind yourself there’s a lot of things in your life that are working
-Write, shoot and direct an image in your head where the future event that you’re worried about works out (I can have it right along with a script where it doesn’t work out but I need to also come up with one where it does work out)
-It is better to think of a positive memory, playing it from beginning to end or think of a desired outcome, playing it from beginning to end
ANTI-ANXIETY MEDICATION
-My therapist recommended visiting my primary care physician and asking for some anti-anxiety medication. I should tell him that I’m stressed and my therapist recommends I take something for my stress during this challenging time
-When I did visit my primary care physician, he agreed and put me on CITALOPRAM (aka CELEXA) – Anti-anxiety medication. It ended up making a huge difference and I wished I had been on it earlier.
-I told therapist that some of the relaxation techniques that I had been doing weren’t working any more. She said that I’ve been traumatized. Of course some of my relaxation techniques won’t work any more because I’m exhausted. I should try some new ones.
-She said that I will get better. I shouldn’t think I’m foolish because I had hope for things that didn’t happen. That’s a self esteem thing.
-I need to build my self esteem and confidence. If someone tries to knock me, I need to stand my ground.
-Negative comments only get under your skin if you don’t have confidence in yourself.
-If I have anxiety about something, it’s because my gut detects an issue. If this happens, I should follow this routine:
-DETECT PROBLEM – DO SOMETHING TO CORRECT IT
-The quicker I can get to “do something to correct it” the less I’ll worry. Plus, just knowing that I’m going to do something to correct it will help reduce the worry.
-I NEED TO BE A FRIEND TO MYSELF – I am too hard on myself. I need to be a friend to myself and treat myself like a friend, instead of being harshly critical all the time.
-I should publicly celebrate my successes
-Although some people go the other way and celebrate themselves too much, I have gone the other way and have made myself invisible. I need to celebrate myself more.
-DOWN TIME – I need to schedule some down time each day so that I relax. It’s not good to be constantly in a hurry. I should set aside time each day to do this and read or watch TV or nap. This is part of being a friend to myself.
WHEN PEOPLE ASK ABOUT MY CONDITION
She said that it’s not appropriate to go into the details. I can just tell them that I’m healing and move on.
END OF THERAPY NOTES
SIX WEEKS SINCE ABCESS DRAIN/ 17 WEEKS SINCE FISSURE SURGERY
STATUS OF ABSCESS/ INFECTION
-I went for a follow up with my surgeon. He probed me with a finger and had me squeeze. He said my strength back there was good.
-SPHINCTEROTOMY WOUND – It’s still healing. There’s a divot there which he says is a good thing. It looks like it’s healing over. He feels it will take 3 to 6 months to see if it heals completely.
-INFECTION – He can’t tell yet if it’s over or not. It doesn’t look bad.
He was happy that he felt a divot there – but he was concerned that when he pushed on the abscess wound, puss came out the other end (rectum). I should continue to watch out for chills, fever, pain, redness, swelling.
-SURGERY – There’s still no verdict on whether I’ll need surgery or not. There’s a 60/40 chance (60 I won’t/ 40 I will) Even if there is a surgery, he says it looks like it will be minor because it looks superficial
-SITZ BATHS – I should just take them after my BMs. I don’t have to take them before I go to bed. They’re just for cleansing mainly. Some soothing. They really don’t help with the healing
-WORKOUTS – I can do push ups. If I work out and I get sweaty, I should make sure that I rinse the area down there afterward.
A week after this, I made a return visit to my primary care physician because of three issues:
STRESS
-My therapist suggested I talk to him about prescribing something to ease my anxiety and stress. He thought it was a good idea. He said that stress and anxiety can definitely lead to a fissure because the constant tightening down there can wear on the area and wear it down. That’s why most of the things to fix a fissure are about easing the tightening down there.
The medicine he prescribes
-He prescribed the anti-anxiety medication CITALOPRAM (aka CELEXA).
-It won’t constipate and won’t stop the healing (In the old days, the medicine would constipate but not any more)
-I should start taking the medicine. It won’t kick in right away. It will probably take a week. I should take one in the morning. They will give me an initial supply of 30 and see how that goes.
-(NOTE: In hindsight, I wish that I had thought to ask about an anti-anxiety medication earlier. Celexa really helped reduce my stress which then helped reduce the hard stool issue that I was having, too. I would continue to take it until the abscess was completely healed.)
MY TONGUE FUZZ
-About a week and a half ago, it started feeling lumpy and the center of it turned black and a fuzz began growing on top. It’s a little better. He checked it out. He says it’s a yeast infection (aka thrush) that was brought on by the anti-biotics that I was taking. It’s a common occurrence. He asked if I was eating yogurt. I told him about all the yogurt that I was eating. Apparently, it wasn’t enough. He’s going to prescribe some stuff.
-He prescribed MYCOSTATIN (aka NYSTATIN)
-It’s a liquid and it’s okay to take it at the same time as the anti-anxiety stuff
-It comes in a bottle. They give you a little syringe like thing that you fill up with about 3cc of Mycostatin (aka Nystatin), then you inject it into your mouth on top of your tongue. You then swish it around for a minute, then swallow (They usually say 3 minutes but nobody can do it that long)
HARD STOOL
-I’ve been getting some harder stool in the morning.
-I’ve been also getting some mucus with it
-He immediately said it was the result of IBS (irritable bowel syndrome)
-Chronic stress can cause mucus and it can weaken the skin down around the anus.
-If I keep having hard stool, I should take MERALEX (a stool softener). Don’t take the amount they recommend. Just add a ½ teaspoon to my prune juice if I need it. It will pull water into my stool. I should take it in small doses. (A quarter cap?) It will probably take 3 to 4 days to work
-IBS goes back and forth between constipation and diarrhea
NINE WEEKS SINCE ABCESS DRAIN/ 20 WEEKS SINCE FISSURE SURGERY
I went back for a follow up with my colorectal surgeon. Here’s what he said:
-He examined me and probed me with his finger. He had me squeeze and said my strength back there was real good.
-It looked like it’s healing. It doesn’t look like there’s an infection.
-Feeling around where the abscess was, he feels something. He thinks it might be scar tissue or possibly a fistula. (If it turns out to be a fistula, I will need surgery)
-I don’t have any symptoms but I should keep watching.
-He didn’t see any drainage. If I should have drainage, I should give him a call and have a return visit. The last time I was there, he saw clear drainage and that’s a sign that it’s healing.
-I might have a little blood back there after he probed me. This is nothing to worry about. It’s just from the probing. (He examined me with his finger, then with a probe)
-It might take 3 to 6 months to see what it will do. The further out you get from it without any trouble, the better it is.
-I told him about the two medicines that primary care physician put me on. (Nystatin and Citalopram)
-SITZ BATHS – I should continue what I’m doing. It seems to be working. It’s mainly for comfort. When drying off afterward, I should spread my cheeks and clean up in there but I don’t need to go up inside.
-If I have a BM at work, I should just make sure I clean the area. I should take my own TOILET PAPER to work because it will be softer. Usually, the toilet paper provided at an office is cheap, rough and scratchy. Using your own toilet paper will save a lot of discomfort if I have to wipe the area a lot.
-There’s nothing else I can do to help it heal. Just keep doing what I’m doing.
-SPHINCTEROTOMY WOUND – It’s still healing. It’s a divet that’s filling.
-Again, the further out from this, the better my chances. It looks good, like it’s healing but I still have to be watchful.
-He wanted to see me in a month. I told him I would be out of town. He said that’s fine (I only need to come back right away if I see drainage)
-I explained what my stool was like (solid but soft enough to coil up). He seemed to think this was fine.
I went back to see my primary care physician to check up on the following:
MY TONGUE
-It still has a black, fuzzy patch. He called it the black hairy tongue.
-He said that the Infectious Disease Center says not to treat it. It’s an imbalance and your body will take care of it.
-He tried to knock it out with the Nystatin. It didn’t work. He told me to stop taking the Nystatin
-He’s going to give me an anti-fungal pill (LAMASIL 250mg)
-I should take it for 30 days then stop
-Hopefully, it should knock it out
ANXIETY
-He wants me to continue taking the anti-anxiety pill until after my fissure stuff is healed.
-He’s giving me a 90 days supply
-The dosage that I’m taking is low enough that I won’t have to taper off when it comes time to stop the medication
-I can take both the anti-fungal and the anti-anxiety in the morning together
-I can take them with food.
-When I run out of the anti-anxiety, I should tell the pharmacy to call my primary care physician and get authorization for a refill.
14 WEEKS SINCE ABCESS DRAIN/ 25 WEEKS SINCE FISSURE SURGERY
I went back for a follow up with my colorectal surgeon. Here’s what he said:
-It looks good. The sphincterotomy is covered. The infection is healed
-He doesn’t feel a tract. There’s no fistula
-You can still get an infection
-Everyone can. It’s like getting a zit. A gland can get clogged like a zit
-There’s just not one at this point
-He thinks the infection occurred after the surgery, not before
-I don’t have to continue the sitz baths. If I do continue, it would just be for comfort.
-After each BM, I should wipe, rinse and dry. I can part the cheeks and dab a little.
-Incontinence – He felt down there and said that I have good strength. It shouldn’t be an issue.
-If I like, I can do sphincter strengthening exercises. I clench the sphincter for 10 to 15 seconds, then release. Do this 10 times in a row each day for however many days I’d likes
-Sweat – If I sweat down there, I should dab it dry. Everyone should. If I can’t get to it for 8 hours, it won’t be a crime. Just get to it as soon as I can.
-After a shower, everyone should make sure they dry down there.
NINE WEEKS LATER…
I went back to see my primary care physician. My anxiety medication (CITALOPRAM 20mg) was about to run out. I had 8 pills left. He suggested I do the following:
-I should stop cold turkey.
-I may feel dizzy for 2 weeks
-It may take a week or so for the medication to get out of my system
-It will take 4 to 6 weeks to see what the psychological change is like
-This will occur about a month and a half from now.
-I should see how it feels and make a judgement
-If I decide to continue going without it, I should let them know that I’m going forward without it
-If the anxiety comes back and I feel that I should go back on it, I can go back on it.
-I would stay on it for a year, then get off it after a year
-It takes about a year of taking the drug for it to change the chemistry of the brain. Once it’s done its’ thing, hopefully, I wouldn’t need it any more and it will have changed my anxiety for the better
-He kept asking me if I thought I had a lot of anxiety before the fissure incident. Without hesitation, I said, “Yes.” He said a lot of people with anxiety get fissures.
-I should call them in a few weeks and let them know if I’m staying off of it or getting back on it.
-At this point, I still have 8 pills left. If the dizzy-ness gets too bad while I’m withdrawing, I can start taking the pills again and slowly ween myself off
-SLEEP – He seemed to think that the CITALOPRAM wouldn’t make me drowsy. It would make me more relaxed and less anxious. This would probably make me less likely to wake up when I should be sleeping
-If I start taking it again, he suggest to take it before bed time and see if I’m still falling asleep again in the morning.
-I can take the pill with prune juice.
-SEX DRIVE – Yes, CITALOPRAM affects sex drive. In fact, they prescribe the same medication for pre-mature ejaculation. If I decide I want an anti-anxiety medication again, they can put me on something that won’t affect the sex drive.
27 WEEKS SINCE ABCESS DRAIN/ 38 WEEKS SINCE FISSURE SURGERY (And almost a year since the fissure started developing.)
I went back for a follow up. He asked me: Am I bleeding? Do I have puss? Am I sore? Chills? Fever? I answered “No” to all of these.
He examined me and said:
-It is healed and the infection is gone
-This maybe the last time I have to visit him
-I told him I was off the anti-anxiety medication and I’m not doing sitz bathes since the last visit
-MUSCLE STRENGTH – He asked me to push. I told him I didn’t do that any more. He said I didn’t have to and he examined any way. He probed me with his finger and told me to squeeze. He said I had good muscle strength. He asked if I had trouble controlling BMs. I told him “No.” I can hold it until I get to the bathroom. I said that every once in awhile I might slip a little gas. He said that it’s normal and probably a result of the surgery.
I told him that sometimes it takes forever to wipe the area clean. Again, he said that it was probably a result of the surgery and normal. He mentioned that I could always have surgery to get rid of the skin tags on the exterior of my anus but he seemed to not want to advise that. I should just live with it.
If I’m worried about the strength down there, I can do the sphincter strengthening exercises. You squeeze and hold for about 10 to 15 seconds and release. Do this about 10 times a night.
-SWEAT – If I sweat after a work out, I should definitely shower and dab the area. If I climb stairs or sweat during the night, I don’t have to freak out. Just clean the area later
-EXERCISE & SQUATS – I told him that I had experienced some pain down there after doing squats while trying to exercise. He said I might have created a small hemorrhoid down there when I did it. Lifting heavy things can pop a hemorrhoid.
It’s natural for your body to create hemorrhoids. It creates them to cushion the BM that come through. The hemorrhoid can go away or they can stay and become trouble. If I get a little red, sore and irritated down there, I can apply some DESATIN (I am unsure of the spelling) People use it to help their kids with diaper rash. I should only use it if I feel I need it. Since there’s no open wound down there, it shouldn’t be a problem.
There are no restrictions on the exercises I can do.
-**NOTE** Later, I came to realize that the scar tissue healed down there and became rigid. When I did certain exercises like sit ups, it would strain the scar tissue and make it sore. So, I stopped doing certain kinds of exercises, adjusted my work out and things were fine.
-FOOD – Not too much RICE, BREAD or NUTS. They can constipate. SPICY FOOD isn’t the best either.
COFFEE is okay. In fact, it can act as a stimulant.
I asked him what I should do to avoid getting a fissure in the future. He said eat plenty of fruits, vegetables, bran. Drink plenty of water.
I asked about things to watch out for and he pretty much told me the same stuff that I already know.
-The nurse said I finally graduated
-I thanked them both for their help and left.
-They said if I have any other issues, I know where I can find them.
A YEAR SINCE MY FIRST DOCTOR VISIT REGARDING THE FISSURE.
31 WEEKS SINCE ABCESS DRAIN
42 WEEKS SINCE FISSURE SURGERY
I’ve been doing really well. No issues. On Monday, 4/29, I worked out with some weights. The next morning, when I had my BM, I noticed some blood on the stool and blood on the tissue. I thought that it might be nothing but I thought I should get it checked out. That night, I had another BM. It seemed to have a few faint traces of blood but nothing much. I did notice that I had a large hemorrhoid that night. It went away the next morning. The BMs that I had since then contain no blood and seemed fine.
My colorectal surgeon checked me out. He felt around, put a scope in and said the following:
-It’s not the fissure or the surgery. That looks fine and it’s not an infection
-There did seem to be a small hemorrhoid but nothing to be too concerned with
-He gave me a prescription for a suppository (HYDROCORTISONE SUPPOSITORY). I should only take it if I’m bleeding again. It contains steroids and I shouldn’t take it forever. It will reduce the swelling of the hemorrhoid.
-Alternating between standing and sitting at work shouldn’t affect the hemorrhoid (In fact, that activity is for other health benefits, fights obesity)
-Exercise – I should avoid my workout for awhile. He thought that any kind of exercise (push ups, weights etc) would probably affect it. It should just hold off for awhile, maybe use small weights. There’s no rhyme or reason why exercise sometimes doesn’t cause hemorrhoids and other times it does.
-He wanted to see me again in 2 months. If everything is okay at that time, I can cancel the appointment.
-After that visit, I didn’t have any issues. I ended up canceling the next appointment because I didn’t need it.
-Once in a while, I would get a little blood with a BM. It wasn’t much but it did alarm me. When I saw this, I would put on a latex glove, lay on my side and insert one of the HYDROCORTISONE SUPPOSITORIES. With the tip of my finger, I would hold it for a few moments. The suppositories melt when in contact with body temperature and they have a tendency to shoot right back out if you don’t hold it there for a few seconds. I would lay on my side for maybe 5 to 10 minutes and let the suppository melt, then I’d get up, dab away the excess liquid and things would be fine.
-The next day, I wouldn’t have any blood.
-As time went on, I took better care of myself.
-I drank plenty of water
-I ate plenty of fiber
-I cut out alcohol and coffee
-Before I went to bed, I would drink a half cup of prune juice, to make passing stool the next morning easier.
-When I woke up in the morning, I would take a large glass of water and drink down a probiotic pill (CULTURELLE). It seemed to help with my digestion and it seemed to me that I stopped having issues with hard stool.
-After awhile, I suspected that part of my issue with hard stool was a bacterial imbalance in my digestive tract. Because of years of abuse and family history, I didn’t have enough good bacteria in my digestive system. That’s why I started taking the probiotic and it seemed to help
-Other good sources of probiotics are yogurt, Kefir (it’s a drink) or sauerkraut. (Although with the Kefir, I did seem to have a few issues. I suspect it might be because of some lactose intolerance. I cut it out and I was fine).
IN REVIEW
-WARNING SIGNS – A warning sign of a potential fissure would be pain down there. That’s when I should see him. (Or trouble going to the bathroom)
-SUPPOSITORIES – HYDROCORTISONE – You need a prescription to get them. You can get an over the counter cream and apply it to the hemorrhoid if you’d like. It’s not as powerful as the suppository but it might do the trick. The purpose of the suppositories is the shrink the inflammation.
-He said that everybody has hemorrhoids. Only some get so bad that they become chronic. You can get them from straining. Weightlifters get them because they are straining so hard. As long as I don’t get into heavy, heavy weightlifting, I should be fine. Just be sure to rinse down there after working out.
-MIRA-LAX – It’s a stool softener. He doesn’t recommend taking it forever. Take only as needed. One long term effect of taking it too long would be that it stains the inside of the colon.
-CITRUCIL – It’s a fiber supplement. It’s fine to take this a long time. It’s just fiber.
-SKIN TAGS – He called them hemorrhoids. If they become an issue, I can have them removed but he doesn’t recommend it if I don’t have to. He can see that they might cause some issues when wiping.
- rockybalboa76
- Fibre Addict
- Posts: 24
- Topics: 2
- Joined: 12 Aug 2014, 14:36
- Has thanked: 0 time
- Been thanked: 14 times
- Gender:

Re: There is hope - LIS and abscess
Thankyou so much for your fantastic detailed posts! Plenty of info for anyone going through LIS


OMB x


OMB x
fissure after hem banding and tag removal feb 11
Pelvic floor therapy
Diltiazem
Botox June 13
Nitro
Internal flap July 14
EUA and polyps removed Nov 14
Diagnosed with neuropathy Jan 15
Diagnosed with HS EDS type 3 (causes poor wound healing )
Pelvic floor therapy
Diltiazem
Botox June 13
Nitro
Internal flap July 14
EUA and polyps removed Nov 14
Diagnosed with neuropathy Jan 15
Diagnosed with HS EDS type 3 (causes poor wound healing )
-

owmybum - Moderator
- Posts: 2851
- Topics: 42
- Joined: 16 Sep 2012, 16:00
- Location: UK
- Has thanked: 205 times
- Been thanked: 159 times
- Gender:

- Mood: UGH !
Re: There is hope - LIS and abscess
Amazing posts, Rocky. Thanks so much for sharing your experiences.


Nifedipine/lidocaine, no help
Diltiazem, effective, but caused major rash
Nitroglycerine, effective.
Topical estrogen for final healing.
Gentle heat to bottom - pain relief, muscle relaxant
Kondremul mineral oil
Time - lots of time.
Status - Healed!
Diltiazem, effective, but caused major rash
Nitroglycerine, effective.
Topical estrogen for final healing.
Gentle heat to bottom - pain relief, muscle relaxant
Kondremul mineral oil
Time - lots of time.
Status - Healed!
-

Scientist2516 - Moderator
- Posts: 1120
- Topics: 16
- Joined: 21 Jul 2013, 16:00
- Has thanked: 157 times
- Been thanked: 214 times
- Gender:

Re: There is hope - LIS and abscess
Thanks for those kind words. I hope the information helps. Remember, it's like Rocky says, "It's not how hard you hit. It's how hard you can get hit and keep moving forward. That's how winning's done." It's a challenge but you will heal. Things do get better. Just don't over think it -- and keep moving forward.
- rockybalboa76
- Fibre Addict
- Posts: 24
- Topics: 2
- Joined: 12 Aug 2014, 14:36
- Has thanked: 0 time
- Been thanked: 14 times
- Gender:

Re: There is hope - LIS and abscess
Thank you for all of the help and information you provided.
Fissure since about 2007
Fissure diagnosed in 2011
Diltiazem for two years - didn't work well
LIS January, 2015
Hemorrhoidectomy December, 2017
Fissure diagnosed in 2011
Diltiazem for two years - didn't work well
LIS January, 2015
Hemorrhoidectomy December, 2017
- chachacha
- Moderator
- Posts: 1118
- Topics: 19
- Joined: 16 Jun 2013, 16:00
- Location: Canada
- Has thanked: 28 times
- Been thanked: 207 times
- Gender:

Re: There is hope - LIS and abscess
I’m commenting so I can come back to refer to this. Lots of good information, thanks.
- Coconutoil
- Salt Bather
- Posts: 50
- Joined: 18 Apr 2020, 17:34
- Has thanked: 0 time
- Been thanked: 8 times
- Gender:

7 posts
• Page 1 of 1
-
- Similar Topics
- Replies
- Views
- Last post
-
-
Is there hope?
by over10yearsnow » 11 Feb 2016, 22:22 in General Anal Fissure Discussion - 5
- 2290
-
by pinpin

28 Mar 2016, 05:29
-
Is there hope?
-
-
A BREAKTHROUGH! there is hope!
1, 2, 3 by Fissurefrustration » 02 Jul 2021, 07:25 in General Anal Fissure Discussion - 20
- 6100
-
by missy moo

08 Oct 2021, 02:53
-
A BREAKTHROUGH! there is hope!
-
-
Are there warning signs of a fistula/abscess?
by sean530 » 04 Dec 2018, 07:08 in FISTULA - Are you having surgery for a Fistula or already had it? - 2
- 2099
-
by Talesofmytail

03 Feb 2019, 16:20
-
Are there warning signs of a fistula/abscess?
-
-
8 weeks after LIS and losing hope
1, 2 by blue_belle » 21 Apr 2019, 14:28 in LIS - Considering surgery or already had it? - 10
- 5031
-
by ken2021

06 Aug 2021, 23:33
-
8 weeks after LIS and losing hope
-
-
Anal fissure story + severe anxiety attacks and losing hope
1, 2 by Severelydepressed » 19 Oct 2015, 09:16 in General Anal Fissure Discussion - 19
- 9860
-
by mada2885

07 Feb 2016, 22:35
-
Anal fissure story + severe anxiety attacks and losing hope
Return to Anal Fissure Success Stories
Who is online
Users browsing this forum: No registered users and 0 guests